This paper attempts to explain the dimensions of India’s chronic malnutrition which continues to afflict infants, children, adolescents and adults, and why it is not decreasing faster. It goes into its historic and generational causes, which have made it evolve into a very multi-causal and complex affliction, the causes of which can broadly be categorized as India’s triple deficit, namely, the dietary deficit, the information deficit and the market deficit. The paper explains each of these deficits and their impact on the nutrition/health status of various age groups, and makes a case that India’s chronic undernutrition and micronutrient deficiency can be reduced with much greater speed and sustainability if the triple deficit is addressed through new and innovative interventions

By Veena S Rao
Retired Secretary to Govt of India
Advisor, Karnataka Comprehensive Nutrition Mission
"Views are personal"
Nourishing India – What Needs To Be Done
India has become quite accustomed to being labelled as home to the largest number of malnourished children in the world, or home to the largest number of undernourished persons in the world. Year after year, leading annual publications appear with the same stark statistics. Very little formal comment comes from government, but there do appear very concerned scientific and social commentaries upon the poor health and nutritional status of a large percentage of our people, urging the government for strong action. However, soon, this critical, complex and elusive subject which forms the foundation of our human capital becomes overshadowed by another priority.It is now over a month since the National Family Health Survey 5 (NFHS 5) first phase was published covering 17 States and five UTs.[i] There are ups and downs – infant and child mortality rates, including perinatal and neo natal mortality rates showed substantial improvement, but nutrition indicators and anemia, especially among children and women have deteriorated. Stunting among children below 5 years has indeed increased drastically in several States, including the more progressive ones, such as, Kerala and Goa and in some of the traditionally better nourished North East States, particularly Meghalaya, Nagaland and Tripura. But Manipur and Sikkim have shown a dramatic decline from 28.9% to 23.4% in Manipur and 29.6% to 22.3% in Sikkim. Even Bihar, a difficult State, has shown remarkable improvement in reducing stunting from 48.3% to 42.9% (with rural data better than the urban data) and Assam too has shown slight improvement. In most other States, except for Telangana, where stunting has increased from 28% to 33.10%, the position appears to be more or less static, with a one percent change this way or that.
The percentage of wasted children in most States has also gone up, the highest increase coming from Ladakh from 9.3% to 17.3%, followed by Nagaland from 11.3% to 19.10%, and Jammu & Kashmir from 12.2% to 19%. Both Bihar and Assam see an increase in wasted children, from 20.8% to 22.9% and 17% to 21.7% respectively. Karnataka has shown remarkable improvement bringing the percentage down from 26.10% to 19.5%.
As far as under-weight is concerned, except for improvement in Karnataka, Meghalaya and Sikkim, in other States the percentages have either have either increased or plateaued.
Again, there has been no comment or response from government or any policy making authority, though several articles by eminent public health/policy experts in both mainstream and social media have appeared expressing deep concern. There will, in all probability be further deterioration in nutrition indicators following the COVID 19 pandemic, in the next phase of NFHS 5 which is currently going on, primarily on account of loss of livelihoods, reduced food consumption among the poor, and dislocation of government nutrition programmes.[ii]
For how long have high levels of malnutrition afflicted India’s population? Let me begin by quoting from the concluding paragraph of Chapter 1 of ‘A brief Survey of the State of the Public Health’ – India’s first comprehensive report on nutrition and health – the ‘Report of the Health Survey and Development Committee’, 1946, headed by Sir Joseph Bhore.[iii]
“To sum up, the factors responsible for the low level of ill-health in India include, among others, the prevalence of malnutrition and undernutrition among appreciable sections of the people, the serious inadequacy of existing provision for affording health protection to the community and a group of social causes consisting of poverty and unemployment, illiteracy and ignorance of the hygienic mode of life and certain customs such as early marriage. The cumulative effect of these factors is seen in the incidence of a large amount of preventable morbidity and mortality in the community. The continued prevalence of such conditions for many generations has probably helped to create in the minds of the people an attitude of passive acceptance of the existing state of affairs. This attitude will have to be overcome and their active cooperation enlisted in the campaign against disease, insanitation and undesirable personal and community habits, if any lasting improvement in the public health is to be achieved.”
The author would like to emphasise that these factors continue to persist in India even today, though in lesser degree, particularly the attitude of passive acceptance of an affliction, which they do not understand why they have.
It is also important to revisit the findings of the food surveys conducted between the years 1935 to 1948. These are adequately quoted and form the basis of the recommendations of the First Five Year Plan, (1951-1956), regarding nutrition in Chapter 32, Paras 25 and 26. [iv]
Para 25 reads as follows: “The average diet of an Indian is lopsided primarily because of its extremely high cereal content. The other noticeable feature is that the diet lacks in adequate amounts of protective foods leading to inadequacy and very often to total lack of proteins of good quality. Inadequacy of minerals and most of the important vitamins in more or less varying degrees is the other important feature. It has not been sufficiently realized that the inadequacy of B group of vitamins is of the most serious import in view of the large intake of carbohydrates. Intake of vitamins A and C also is often inadequate”. These surveys have led to the following observations: “It appears that two-thirds of the families did not consume any fruits and nuts at all. About one-third of the families did not consume sugar and jaggery, meat, fish or flesh foods, and a quarter of the family groups did not consume milk and milk products or leafy vegetables. Again, amongst the groups of families consuming particular foodstuffs the intake of leafy vegetables, other vegetables, ghee and vegetable oil and pulses was below the desired or recommended level. Only in about one-fifth of the groups of families surveyed was the intake of pulses and other vegetables up to the recommended level. Though any generalisation on the data presented is not desirable for reasons more than one, yet it may be stated that in about four-fifths of the families surveyed the intake of protective foods was either nil or below standard.
Para 26. “The bulk of the population cannot afford to purchase a satisfactory diet. In terms of average income it would hardly be possible for more than 30 per cent of the population to feed themselves on an adequate scale” (First Five Year Plan, 1951-56 Chapter 32).
The reports and data referred to above clearly establish that India has a long, generational history of chronic malnutrition. Undernutrition and micronutrient deficiency which even today afflict around fifty of our population, is not something that was suddenly acquired because of successive natural calamities, food shortages or war. Clearly, it is one of the outcomes of sustained socio-economic deterioration caused by the increasing poverty in the 19th and 20th centuries under colonial rule, brought about by changed occupations and agricultural patterns enforced by colonialism, and surging illiteracy resulting from depriving the existing and flourishing indigenous system of education of patronage and funds. Reduced incomes, poverty, compounded by rapidly growing illiteracy, poor health care, and lack of opportunity for upward economic or social mobility, created the most fertile environment for chronic malnutrition and micronutrient deficiency among the general population of India, the remnants of which persist even today.
In 1947, independent India was born with a meagre per capita income of Rs 249.6, a literacy rate of 18.33% (with female literacy at 8.86%)[v] male and female life expectancy at 26.91 and 26.56 years respectively, a death rate of 22.8 per 1000, infant mortality rate of 158 per 1000, and maternal mortality at 20 per 1000 live births, with only one third of the population having the income to feed themselves adequately.[vi]
With this background, India’s malnutrition in today’s context, (which refers here to calorie-protein- micronutrient deficiency only) has evolved as an extremely complex biological condition with multiple and heterogeneous causes, multiple manifestations, and an inter-sectoral, inter-generational character. It is the hidden layer of ill-health, poor physical and cognitive growth which leads to poor learning skills in children, and eventually to lesser income earning capacity in adults, and perpetuation of the poverty cycle.
Poverty is a prominent, but not the sole cause of malnutrition. While all malnourished people may not necessarily be poor, people who are poor would generally be malnourished. The fact that the percentage of people suffering from undernutrition and micronutrient deficiency exceeds the percentage of people below the poverty line clearly establishes that undernutrition has multiple other causes.
These can be clubbed as follows:
Physical Causes– such as, poverty, hunger, under-nutrition, calorie-protein-micronutrient deficit in daily diet, infection and disease.
Historic and Socio-economic Causes- such as, generational poverty and low income caused by illiteracy/low literacy and lack of skills; gender discrimination which became embedded in social custom, and lack of information and awareness.
Behavioural and Socio-cultural – arising out of poverty, gender discrimination, lack of information and awareness and superstition, leading to low status of women; lesser food and health care for the girl child within families; early marriage of girls, early/frequent pregnancies, inadequate weight gain during pregnancy; delayed complementary feeding to infants – in short, negative child care and feeding practices, ignorance and neglect of adolescent and maternal care, lack of knowledge regarding the best balanced diets within scarce family budgets, all cumulatively resulting in the inter-generational cycle of malnutrition.
Governance related Causes – such as, lack of intensive grassroots Information Education and Communication (IEC) programmes which provide families and communities information and awareness regarding the importance of balanced diets within their purchasing power, regarding proper child, adolescent and maternal care; inadequate nutrition/ health interventions and poor coverage at grassroots level for women, adolescents and children, especially in chronic malnutrition areas; coverage gaps in safe drinking water and sanitation programmes; lack of real time, action based nutrition monitoring and surveillance; and lack of accountability of programme managers regarding persisting poor nutritional indicators among communities. (There is not merely a lack of clarity, but even lack of demand for accountability as to who exactly in the governmental system, should be held accountable for the continuing high rates of malnutrition in India, particularly increased wasting among children, as reported in National Family Health Survey 4 (NFHS 4) 2015-2016.
Critical interventions to address these heterogeneous, root causes at the programmatic level can be clubbed as follows: [vii]
- Specifically targeting the inter-generational cycle of malnutrition by simultaneous addressing the nutritional needs of infants, children, adolescent girls and pregnant and nursing mothers.
- Bridging the calorie-protein micronutrient deficit in the daily diets among the inter-generational target groups by providing appropriate energy dense fortified supplementation for consumption.
- Bridging the Information Gap through a sustained, multi-layered general public awareness campaign, most importantly through interpersonal communication to reach the general public, especially in households, regarding proper nutritional practices within existing family budgets, and proper child, adolescent and maternal care, and for creating demand for on-going government programmes.
- Accelerating, integrating and tightly monitoring multi-sectoral ongoing programmes that have impact on malnutrition, such as, Immunization and Vitamin A Supplementation, Anaemia Control, Water and Sanitation, etc. and achieving convergence between the ongoing programmes so that they operate simultaneously, and filling programmatic gaps. Involvement of the community, Non-Governmental Organizations (NGOs), women’s self-help groups (SHGs – village organizations for women) and village panchayats (elected village councils) for intensifying demand creation and increasing programme coverage.
- Real time monitoring of the beneficiaries’ nutrition indicators, particularly regarding underweight, stunting and wasting of children, body mass index of adolescent girls, pregnancy weight gain, and incidence of low birth weight babies
India’s malnutrition and the Triple Deficit
The author believes that India’s chronic undernutrition and micronutrient deficiency is perpetuated by three deficits – the dietary deficit, the information deficit and the market deficit.
Dietary deficit, that is, the protein-calorie-micronutrient gap which exists in the daily diets of at least fifty percent of the people, is the most proximate and direct root cause of chronic under nutrition in India.
India is proud of its demographic dividend that 67.3% of its population is between 15-59 years of age, and that this demographic advantage of having a young working population will persist for at least another three decades.[viii] This factor is emphasized at most social and economic fora, and is seen as India’s comparative advantage vis a vis several other industrialized countries.
However, a critical factor which has not yet been stated or acknowledged in contemporary public policy debate or in nutrition/health focused debate is that the potential of at least fifty percent of our demographic dividend to access the best opportunities to rise above poverty and contribute to the economic growth is severely handicapped on account of under-nutrition, poor health and morbidity, because of generational and routine dietary deficit within their daily diets.
What exactly is Dietary Deficit, and what impact does it have on the lives of children, women, adolescents and adults?
According to the FAO publication ‘Undernourishment around the world, Depth of hunger: how hungry are the hungry?[ix], the depth of hunger, or food deficit, is measured by comparing the average amount of dietary energy that undernourished people get from the foods they eat with the minimum amount of dietary energy they need to maintain body weight and undertake light activity. The greater the deficit, the greater the susceptibility to nutrition-related health risks. A weak, sickly person cannot fulfil his or her individual potential. A nation of weak, sickly people cannot advance.
The diets of most of the 800 million chronically hungry people lack 100-400 kilocalories per day. Most of these people are not dying of starvation. Often they are thin but not emaciated. The presence of chronic hunger is not always apparent because the body compensates for an inadequate diet by slowing down physical activity and, in the case of children, growth. In addition to increasing susceptibility to disease, chronic hunger means that children may be listless and unable to concentrate in school, mothers may give birth to underweight babies and adults may lack the energy to fulfill their potential.’
The World Bank adds that “the depth of hunger is low when it is less than 200 kilocalories per person per day, and high when it is higher than 300 kilocalories per person per day.” [x]
Impact of Dietary Deficit, Hunger and Undernutrition
On pregnant women and new-borns
An undernourished and anaemic pregnant woman, whose diet before or during pregnancy is inadequate, and has gained inadequate weight during pregnancy carries undernutrition to the womb. This will result in growth retardation of the foetus and the infant will be born of low birth weight. Low birth weight increases neonatal and infant morbidity and mortality, retards emotional and intellectual development and leads to permanently stunted height.[xi]
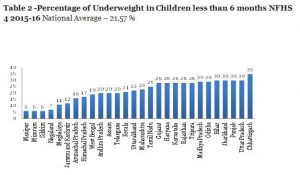
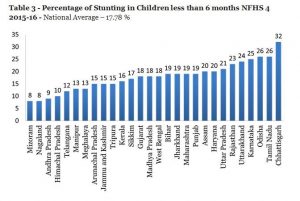
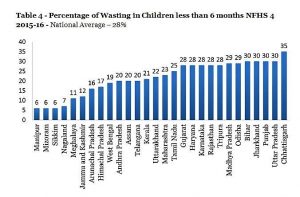
As per the National Institute of Nutrition (NIN) publication, Dietary Guidelines for Indians – A Manual, “composition of breast-milk depends to some extent on maternal nutrition[xii]. Though in general, even the undernourished mothers can successfully breast-feed, in the case of severe malnutrition, both the quality and quantity of breast-milk may be affected, particularly the fat content. Concentration of water-soluble vitamins as well as fat soluble vitamin A (beta-carotene) is influenced by the quality of the maternal diet.” This could also explain the high rate of undernutrition, wasting and stunting of children below 6 months as shown in Tables 2 to 4 below.
On children of six months to 2 years
Undernutrition and anaemia among this age group results in slower physical and cognitive growth, inability to achieve their complete physical and cognitive potential, lower immunity and higher infections, and permanent stunting. Scientific evidence establishes that inadequate nutrition among infants below three years, which is a period of rapid growth of their brain cells, can result in slower and lesser development of cognitive ability.
On school going children and adolescents
Undernutrition, anaemia and micronutrient deficiency among this age group again results in slower growth, reduced ability to learn, play and do physical work. This translates into lower educational achievement as they grow, school dropouts, lesser ability to acquire professional skills and lower income generation capacity as they enter the work force. Additionally, undernourished adolescent girls will become undernourished and anaemic mothers, thereby perpetuating the intergenerational cycle of undernutrition and poverty.
On Adults
Dietary deficit, chronic energy deficiency (CED) and anaemia in adults results in reduced energy to work and earn, thereby making upward mobility difficult and confining them in the poverty trap. The body of such adults suffering from undernutrition and CED becomes programmed to function in scarcity, creating a negative balance where muscles don’t build and existing muscles become thinner. This adversely affects the protective mechanisms of the body and reduces immunity and life expectancy.
Data on India’s Dietary Deficit
Let us look at some data which measures the extent of dietary deficit among the population. Below is some of the data published over the last decade regarding the calorie-protein- micronutrient deficit that afflicts the diets of various age groups of India’s population.
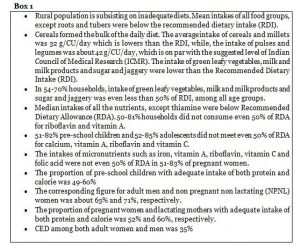
Findings of the National Nutrition Monitoring Bureau (NNMB) 3rd Repeat Survey (2012)[xiii] 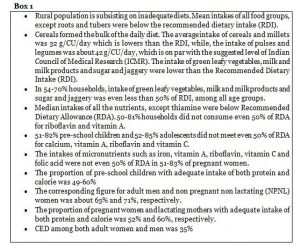
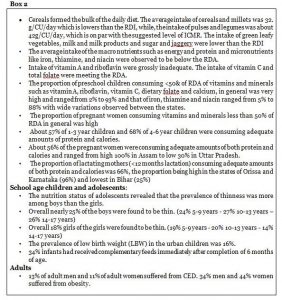
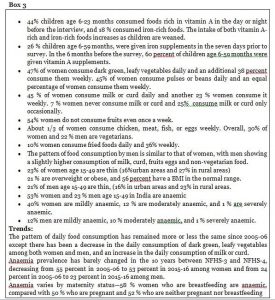
Findings of the National Nutrition Monitoring Bureau (NNMB) Report 2017[xiv]
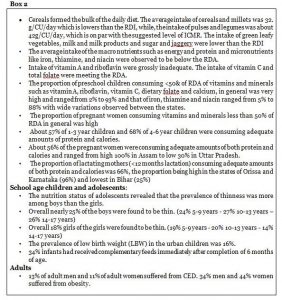
The primary objective of the NNMB Technical Report 27 was to assess the diet and nutritional status of the urban population. This would also include as a secondary objective an assessment of the current status of food and nutrient intake among different age/sex/physiological groups of the urban population in the 16 NNMB States.
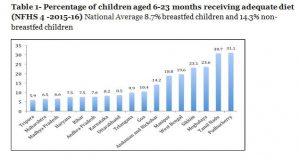
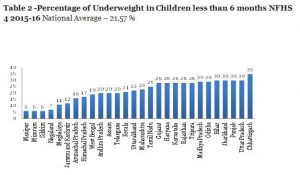
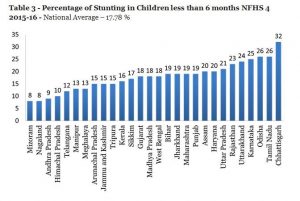
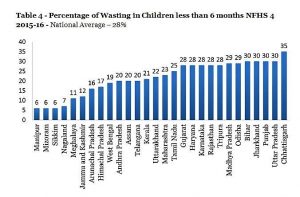
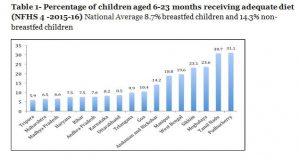
Findings of National Family Health Survey (NFHS 4), 2015-16[xv] 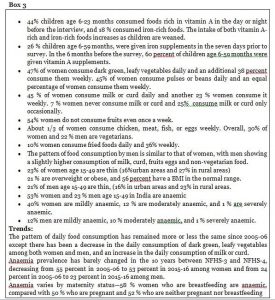 The most graphic indicator of a severe and chronic dietary deficit among mothers and children is given in the Tables below based on data from NFHS 4.
The most graphic indicator of a severe and chronic dietary deficit among mothers and children is given in the Tables below based on data from NFHS 4.
The Tables inform that only 8.7% breastfed children and 14.3% non-breastfed children between 6 to 23 months received an adequate diet. This is the most direct evidence of dietary deficit among infants from 6 months to 2 years. This is an extremely serious indicator which is the source of under-nutrition in the life cycle of India’s afflicted population.
The data goes on to give some more disturbing figures, namely, that 17.78% children below 6 months are stunted, 21.57% children are underweight and 28% are wasted. This data is presumably related to low birth weight (20% NFHS 4) and is a direct indicator of an unacceptably high dietary deficit during pregnancy resulting in poor maternal nutritional status and inadequate pregnancy weight gain. Even more disturbing is that the percentage of children aged 6-8 months receiving solid/semisolid food and breastmilk in India has decreased from 52.6% in NFHS-3 (2005-06) to 42.7% in NFHS-4 (2015-16).
A Feasibility Study of Introducing Low-Cost Fortified Energy Food in India conducted by Karnataka Comprehensive Nutrition Mission (KCNM) in 2018 through KPMG confirms that the dietary intake of calories, protein, fat, calcium and iron is inadequate indicating a minimum gap of 30% in dietary intake in comparison to the recommended dietary allowance, among households earning less than Rs 60,000 per month, particularly among those earning below Rs 30,000/- per month.[xvi]
The study was spread across five states — Karnataka, Odisha, Uttar Pradesh, Gujarat and Maharashtra. Empirical evidence for the study was captured from stakeholder groups on the demand side covering households, doctors, nutritionists and frontline workers (ASHAs-Accredited Social Health Activists and AWWs-Anganwadi Workers/Childcare Centre Workers) as well as on the supply side covering manufacturers, distributors and points of sale such as kirana (general) stores, village haats (weekly markets) and pharmacies to assess the feasibility.
The study observed that 70% of the respondent group subsists on diets consisting mostly of plant-based foods, with low nutrient bio-availability, making access to Fortified Energy Food essential to meet the RDA requirements in the diet. The study also gave a firm finding that there is a direct correlation between high incidence of low weight, stunting and wasting among children; low body mass index and stunting among adolescents, and lack of low-cost Fortified Energy Food in the market.
Bridging the Dietary Deficit – How do we do it?
Addressing the wide calorie-protein-micronutrient gap that exists in around 50% of India’s population, as is indicated in the data provided above, should be stated as a high priority for the Government, if India is serious about reducing undernutrition and micronutrient deficiency. This is also help in achieving the objective of the Poshan Abhiyaan,[xvii] (Nutrition Mission announced by Government of India in December 2017) and for achieving Sustainable Development Goal 2 which aims to “end all forms of hunger and malnutrition by 2030, making sure all people – especially children – have sufficient and nutritious food all year.”
Article 47 of the Constitution of India under the Directive Principles of State Policy casts a constitutional responsibility on Government in this regard:
“Duty of the State to raise the level of nutrition and the standard of living and to improve public health – The State shall regard the raising of the level of nutrition and the standard of living of its people and the improvement of public health as among its primary duties and, in particular, the State shall endeavour to bring about prohibition of the consumption except for medicinal purposes of intoxicating drinks and of drugs which are injurious to health.”
The author believes that there are three minimum essential interventions through which India can start bridging the calorie-protein-micronutrient gap. Each intervention carries its own impact individually, and the collective impact of all three can create a significant improvement in the dietary intake of the people within a short period of time and improve their nutritional status:
A. Bridging the Dietary Deficit by IEC, Behaviour Change and Government Programmes
Bridging the dietary gap can be achieved to a considerable extent through a national Information Education and Communication (IEC) and nutrition awareness campaign, which should be multi-layered and should focus on bringing about behaviour change at the household and grassroots level for educating mothers, families and communities about the importance of simple, basic and essential nutritional practices, mainly:
-balanced diets with locally available, affordable foods within their resources
-proper birth weight of infant, the required weight gain during pregnancy and how to achieve it through additional dietary intake
-exclusive breast feeding for 6 months and starting adequate and appropriate complementary feeding after 6 months
-hygiene, sanitation, safe drinking water and its storage
-complete immunization of children and diarrhoea management
-proper nutritional care of adolescents and nursing mothers
-prevention of anaemia among children, women, adolescents and adults
-breaking the inter-generational cycle of malnutrition.
Such a grassroots behavior change campaign would provide simple but critical information at the household level and would bring about the required behaviour change in families in the remotest habitations of India. This grassroots IEC strategy has been successfully applied and field tested in the World Bank funded Karnataka Inter-Sectoral Nutrition Pilot Projects led by the KCNM, and implemented in two most backward areas of Karnataka State – Chincholli and Devadurga Blocks of Kalaburgi and Raichur Districts. The strategy resulted in positive behaviour change and considerably improved the nutritional status of the beneficiaries.[xviii]
Unfortunately, in spite of a wide information/awareness deficit which exists at household level, especially among lower income families, which is also a major cause for the dietary deficit, India has no comprehensive national or state IEC programme at village level that directly targets households to bring about the required behaviour change. IEC and behaviour change have been highlighted in all our early Five Year Plans, but somehow, successive governments have not been able to make it happen.
India has a vast pool of human resources, particularly women, available at the village level, such as, SHG women, village panchayat women members, NGO field workers, CSR (Corporate Social Responsibility) field workers. The author believes that they can be mobilized, trained, and provided proper IEC material, for conducting the grassroots IEC programme as village nutrition volunteers, (VNVs) and monitoring the results. Such an IEC programme will complement and strengthen the existing government programmes, particularly the Integrated Child Development Services (ICDS), through using existing women SHG resources and would not require any further recruitment by Government.
This experiment of VNVs being agents of behaviour change at the household level through a simple, sound and multi-layered IEC campaign has been tested in the Karnataka Multi-sectoral Nutrition Pilot Projects and has proved successful in bringing about the required behavior change and resulting in improved nutritional status.[xix] The first year of this project focused only on IEC at family and community level, mainly through inter-personal counseling, without any dietary supplementation.[xx] According to data for this period, there was a decrease in undernutrition among all age groups by around 30%. Positive behavior change and higher nutritional and health awareness at household level has been validated in the Impact Assessment conducted by the National Institute of Nutrition.[xxi]
However, it would be important to note that the extent of the dietary gap that is bridged by IEC is to a large extent related to cash availability in the family. In families with higher expendable incomes, IEC provides information and enables the family to bridge the dietary gap through higher spending on locally available nutritious and protective foods. In families with lesser income, the effect of IEC on improving nutritional status, though substantial, is limited by purchasing power, particularly in an inequitable market situation where no low-cost protective or fortified energy-protein foods are available.
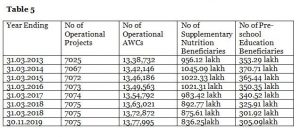
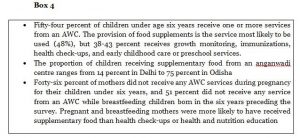
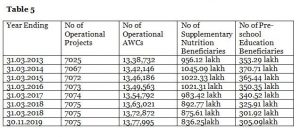
What also becomes quite clear is that the existing supplementary nutrition programmes in India, mainly the Integrated Child Development Services programme, (ICDS) which was announced in 1975 to directly address dietary deficit among children below 6 years, and pregnant and lactating mothers, has not been successful in completely addressing the protein-calorie-micronutrient deficit. The programme appears to have turned stagnant with decreasing coverage, particularly for nutrition interventions, as the tables below clearly indicate.
As per the Annual Report of the Ministry of Women and Child Development 2019-20, the coverage under ICDS and trends since March 2013 are in the Table placed below[xxii]
NFHS 4 2015-16: Findings regarding the utilization of ICDS services in respect of supplementary nutrition and THR (Take Home Ration) are in the Box below: [xxiii]
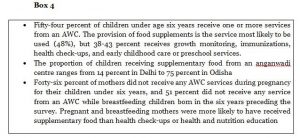
The above data indicates that supplementary nutrition coverage by the ICDS programme is grossly inadequate. This can perhaps be explained by several reports which appear periodically in newspapers all over the country about the poor quality of THR, and therefore it is not consumed by the beneficiaries.
B. Bridging the Dietary Deficit by making accessible low-cost nutritious blended food to all sections of the population in the open market.
One of the major contributing factors of undernutrition and calorie-protein-micronutrient deficiency among large sections of India’s population, especially the poorest 30-40 percent, is that there is presently a complete vacuum in the market for low cost, fortified energy foods for lower income families, who are most vulnerable to malnutrition.
The daily diets of the poorest families are meagre and can at best qualify as subsistence diets. For lack of money and knowledge, the families are not able to provide the balanced nutrition required for healthy growth of children and adolescents during rapid growth periods, for women during pregnancy and lactation, for all age groups of both genders during or after illness, and complementary food for infants after 6 months of age. The nutritional status of adolescent girls and boys are also be a cause for serious concern. Forty seven percent of adolescent girls aged 15–19, the future mothers, are underweight, with a body mass index of less than 18.5, as per the UNICEF State of the World Children Report 2011[xxiv]
At the macro level, even though the per capita income has more than quadrupled in the last decade, the vast dietary deficit remains in terms of protein, calorie and micronutrients among around 50% of our population of both sexes and all age groups, despite the ICDS and Midday Meal Programme having been in operation for more than the last four and two decades respectively.
In spite of the policy prescriptions contained in the National Nutrition Policy 1993 and the National Plan of Nutrition 1995, sadly, the Indian market today is completely inequitable regarding the availability of low-cost energy food for the lower income vulnerable groups. While there is abundance of high-cost ready to eat fortified nutritious food available for all age groups for the affluent, there is a complete absence in the market of affordable, low-cost energy food for the lower income families. The Feasibility Study conducted through KPMG in 2018 under the Karnataka Multi-sectoral Nutrition Pilot Projects,[xxv] calculates a market demand of 42 million tons of low-cost energy food per year, but strangely, no private entrepreneurs want to enter this field. One wonders why, in spite of the specific mandate of the National Nutrition Policy 1983 and the National Plan of Action on Nutrition 1995.
The Global Nutrition Report 2020[xxvi] in its Spotlight Section emphasizes that the high cost of nutritious foods for populations most at risk of undernutrition is a major barrier to resolving undernutrition and warrants urgent policy attention.
The incidence of severe child malnutrition and wasting and its improvement was an indicator which was rigorously monitored by the author on a real time basis in the Karnataka Multi-sectoral Nutrition Pilot Projects It was seen that all cases of severely malnourished/wasted children were from households where both parents were engaged in construction or agricultural labour. The infants were left under the care of elder siblings or grandparents, and apart from some roti, (flat bread made from wheat) rice and pulses, which the infants could not eat, there was no other food in the house. And there was no low-cost children’s food available in the market.
Availability of affordable, fortified energy food in the market assumes even greater importance during the COVID 19 pandemic – lockdown and post lockdown. Reports from the field categorically inform that poor rural families are on a survival diet of rice and wheat given under PDS (Public Distribution System which gives subsidized food grains to low-income families), and sometimes some dal. In many villages, even now there is no milk or any other food for children. A study done by Azim Premji University confirms this.[xxvii] In these circumstances, it is inevitable that there will be a further deterioration in the dietary gap of the poorest sections of our population, a surge in underweight, stunting and wasting among children, poor maternal weight gain and low birth weight babies, higher anemia among children, women adolescents and adults, and lower adolescent BMI (Body Mass Index) during lockdown and post lockdown period.
What India should do
The dietary deficit which is prevalent in varying degrees among the population, as shown in Boxes 1, 2, 3, 4 above, has not yet been acknowledged or articulated by the Government and policy makers as one of the major root causes of chronic and persistent under nutrition and micro nutrient deficiency in India. The Poshan Abhiyaan announced in December 2017 does not contain any reference to it. Neither does the Niti Aayog publication ‘Nourishing India: National Nutrition Strategy, Government of India.’[xxviii] Unless this dietary gap is bridged, large sections of India’s population, particularly the present and future demographic dividend, will forever be deprived of achieving their full physical and cognitive potential. Children’s literacy and numeracy skills will suffer, employability and upward mobility of adolescents and adults in the emerging world economy will remain elusive, and they will remain confined within the poverty trap. Cumulatively, this will result in an appreciable loss of GDP (Gross Domestic Product) to the nation through lost Disability-Adjusted Life Years (DALY) something that has been calculated in numerous studies over the last few decades. The mindset of policy makers and programmers, down to field workers and families, that subsistence/survival diet equals food security must change.
The political executive and policy makers must also note that unlike in the case of outbreak of infectious diseases for which there is an immediate public demand for government intervention, in the case of malnutrition, which is neither visible nor infectious, there will not be any popular demand from the community to address it, as they lack awareness and information regarding their own affliction or its causes. All they know is that they are poor, get tired easily, and their children fall ill often. Hence, in the Indian context it becomes the responsibility of the government/civil society to first provide information and awareness to the community about malnutrition and its causes, and then implement programmes to address those causes.
Government could start showing its seriousness by examining the present nutrition related programmes, and why they are not able to reduce malnutrition faster; whether they are adequate, or require a complete overhaul; should additional interventions be introduced in pockets of chronic malnutrition in every State, which are identified as Aspiration Districts and High Burden Districts – surely, there should be different norms and more intensive interventions in addition to ICDS for these chronically malnourished pockets with the poorest indicators; how does the government plan to address adolescent malnutrition (our future demographic dividend) which is as alarming as child malnutrition, for which we have no clear strategy in place yet. And finally, government must inform us whether the National Nutrition Policy 1993[xxix] is still alive or not, and whether there are any plans to update it, and prioritize interventions in accordance with latest surveys and research findings.
Acknowledging the dietary deficit should be of top priority, because only after there is acknowledgement of it, can discussions take place and a policy be formulated and put in place to address it. The discussions should include the very vital question, whether our present interventions are addressing the root causes of malnutrition in India, what the author has described as the Three Deficits. Clearly, data indicates that India’s current interventions are not able to bridge them, and unless this is done, rapid improvement in its nutritional indicators will not happen.
What is urgently required is a robust grassroots communication strategy to target the information deficit, better coverage by government programmes to address the dietary deficit, and proactive engagement with the food industry, private, cooperative and government, to bridge the market deficit. Public health experts and policy makers are also aware that unless the dietary deficit is addressed, the impact of other nutrition and health interventions will remain sub-optimal.
Bridging the dietary and information deficit and increasing/ improving nutritional intake of the population, as suggested above, does not require heavy financial investment from government. It can be done by intelligently and innovatively creating an implementation model by using existing financial allocations from ongoing national programmes covering women SHGs, panchayats, livelihoods, skill development etc. and piloting it in a few chronic pockets of malnutrition, the Aspiration Districts, which require additional and more intensive interventions. This is exactly the kind of convergence that the Poshan Abhiyaan seeks to achieve.
The COVID 19 pandemic and its unpredictable duration and disruption of existing nutrition programmes and supply chains has created a further nutritional crisis, the ramifications of which are already being manifested. It is now timely and appropriate for government to engage with the food processing sectors and in accordance with the National Plan of Action on Nutrition 1993, incentivize startups for producing low cost energy food for the open market.
It is also important that government partners and stakeholders, domain experts, national and international agencies, donors and philanthropies working in this field, must also acknowledge this serious dietary deficit when they are preparing their India strategy and plans, and integrate interventions to address this in a holistic framework within their mandate, whether it is food fortification or hand washing. This will only enable them to enhance the outcomes that they are working towards within their mandates. Calories, protein and micronutrients, which are fundamental to nutritional status for any strategy, have no substitute.
Raising the diet of our people from subsistence level to higher levels of nourishment through overcoming the triple deficit is the only way we can improve nutritional indicators of our population – children, adolescents and adults. The government must show its seriousness and start addressing this issue urgently through new ideas and innovation
References
[i] National Family Health Survey 5, http://rchiips.org/nfhs/factsheet_NFHS-5.shtml
[ii] https://cse.azimpremjiuniversity.edu.in/wp-content/uploads/2020/06/Compilation-of-findings-APU-COVID-19-Livelihoods-Survey_Final.pdf
[iii] https://www.nhp.gov.in/bhore-committee-1946_pg
[iv] (First Five Year Plan, 1951-56) https://niti.gov.in/planningcommission.gov.in/docs/plans/planrel/fiveyr/1st/welcome.html
[v] (Data from National Commission on Population),
[vi] (First Five Year Plan, 1951-56) https://niti.gov.in/planningcommission.gov.in/docs/plans/planrel/fiveyr/1st/welcome.html
[vii] Karnataka Comprehensive Nutrition Mission- Strategy Paper http://www.karnutmission.org/Strategy%20Paper-%20KARNATAKA%20COMPREHENSIVE%20NUTRITION%20MISSION.pdf
[viii] https://censusindia.gov.in/Vital_Statistics/SRS_Report_2018/SRS_Statistical_Report_2018.pdf – Page 12
[ix] Undernourishment around the world, Depth of hunger: how hungry are the hungry? http://www.fao.org/3/x8200e/x8200e03.html
[x] https://datacatalog.worldbank.org/depth-hunger-kilocalories-person-day
[xi] ‘Undernutrition in Adults and Children: causes, consequences and what we can do’ by Ann Burgess MPH* Nutrition Consultant and Dr Louis Danga MBBS** Paediatric Registrar, Juba Teaching Hospital
[xii] DIETARY GUIDELINESFOR INDIANS-A Manual Page 27 https://www.nin.res.in/downloads/DietaryGuidelinesforNINwebsite.pdf
[xiii] NNMB 3rd Repeat Survey, 2012 covering rural household in the States of Kerala, Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Gujarat, Madhya Pradesh, Orissa, West Bengal and Uttar Pradesh. The average family size was 4.9. The average monthly per capita income (PCI) was Rs.1,356/- at the current rupee value http://maternalnutritionsouthasia.com/wp-content/uploads/NNMB_Third_Repeat_Rural_Survey___Technicl_Report_26.pdf
[xiv] NNMB Technical Report Number 27, 2017, A Brief NNMB Urban Report covering urban households in the States of Andhra Pradesh, Gujarat, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Orissa, Tamil Nadu, Uttar Pradesh,West Bengal, Assam, Andaman and Nicobar Islands, Bihar, Rajasthan, Puducherry and New Delhi. The average family size was 4.3. The average monthly per capita income (PCI) was Rs. 4,941/- https://www.nin.res.in/downloads/NNMB%20Urban%20Nutrition%20Report%20-Brief%20report.pdf
[xv] NATIONAL FAMILY HEALTH SURVEY (NFHS-4) 2015-16 http://rchiips.org/NFHS/NFHS-4Reports/India.pdf Page no: 299- 303
[xvi] A Feasibility Study of Introducing Low Cost Fortified Energy Food in India through Private Sector Participationhttp://karnutmission.org/documents/New_Feasibility_Study.pdf
[xvii] https://pib.gov.in/newsite/PrintRelease.aspx?relid=174025
[xviii] Karnataka Multi- Sectoral Nutrition Pilot Project- A unique communication strategy http://karnutmission.org/documents/KMSNPP_Report_26DEC18.pdf
[xix] How nutritional volunteer workers have taken the lead in tackling high rates of childhood malnutrition in India – The BMJ
[xx] http://karnutmission.org/documents/KMSNPP_Report_26DEC18.pdf
[xxi] Impact Evaluation of Karnataka Multi-Sectoral Nutrition Pilot Project
ICMR- Indian Council of Medical Research, NIN- National Institute of Nutrition- 2019 http://www.karnutmission.org/documents/IMPACTEvaluation.pdf
[xxii] Annual Report 2019-20, MINISTRY OF WOMEN AND CHILD DEVELOPMENT,Government of India. Page no: 30 https://wcd.nic.in/sites/default/files/WCD_AR_English_2019-20.pdf
[xxiii] NATIONAL FAMILY HEALTH SURVEY (NFHS-4) 2015-16- Page No: 260 http://rchiips.org/NFHS/NFHS-4Reports/India.pdf
[xxiv] State of the World Children Report 2011 – Page 21- https://www.unicef.org/sowc2011/pdfs/SOWC-2011-Main-Report-chapter-2_12082010.pdf
[xxv] http://karnutmission.org/documents/New_Feasibility_Study.pdf
[xxvi] https://globalnutritionreport.org/reports/2020-global-nutrition-report/ Page 84-85
[xxvii] https://cse.azimpremjiuniversity.edu.in/wp-content/uploads/2020/06/Compilation-of-findings-APU-COVID-19-Livelihoods-Survey_Final.pdf
[xxviii] https://niti.gov.in/writereaddata/files/document_publication/Nutrition_Strategy_Booklet.pdf
[xxix] http://wcd.nic.in/sites/default/files/nnp.pdf