In Kenya, maternal deaths account for 14% of all deaths to women aged between 15-49 years according to the Kenya Demographic and Health Survey (KDHS, 2014). Neonatal mortality rate stands at 22 deaths per 1000 live births, a proportion calling for urgent action. The number of children dying in the country is used as a marker of social well-being and national development. It is a reflection of the country’s healthcare system and can be used to evaluate the health policies. Like many other health indicators, the burden of maternal and newborn mortality is heaviest among the poor. In the context of urban informal settlements, indicators such as low use of health services and increasing child mortality suggest that the urban poor are a highly vulnerable and marginalized group. Also, with 17 women dying daily in the country during childbirth, all efforts should be directed towards targeted solution finding and implementation of a sound maternal health system. Toto Care Box Africa Trust is a non-profit organization making great strides in bettering maternal health outcomes for poor and underserved women in the Kenyan informal settlement areas since 2016. To date the organization has been able to secure the lives of more than 5000 women and newborns including the poor, those living with HIV/AIDS and the homeless. Additionally the organization has stimulated partnerships in the healthcare system by incorporating the work of various health facilities and corporates in the fight against maternal and newborn deaths. Every mother matters and each newborn deserves a dignified and equal start to life

By Reagun Andera Odhiambo
M & E and Grants Officer at Toto Care Box Africa Trust
Toto Care Box: Enhancing Maternal and Newborn Health in Kenya

INTRODUCTION
The state of maternal and newborn health in the Kenyan context
Kenya, just as other low-and-middle income countries of the Sub-Saharan Africa continues to realize modest maternal and newborn health outcomes. Sub-Saharan Africa had the highest Neonatal Mortality Rate (NMR) globally in 2018 at 28 deaths per 1000 live births according to the World Health Organization (WHO). A number of factors can be directly linked to these outcomes which are often marked with loss of lives, high maternal and neonatal morbidities and other life-long consequences on the lives of the affected.
In Kenya, the recommended and ideal maternal and newborn care remains only available for the elites and those in the high socio-economic class; those who can pay for health services. The remaining majorities only seek basic care in order to survive and are thus predisposed to poor maternal and newborn health outcomes which may lead to preventable deaths and morbidities. Worse even, some shun from seeking basic healthcare for reasons of poverty and stigmatization; they depend on fate for survival. In Kenya 39,000 newborns die annually due to preventable causes. Also, 17 women die daily during childbirth due to lack of lifesaving education. There is urgent need for all efforts to be directed towards curbing this preventable problem endemic in our country.
MAJOR GAPS IN MATERNAL AND NEWBORN HEALTH IN KENYA
The unacceptably high maternal and newborn mortality rates in Kenya relate to a number of factors which should form the basic action points for preventive solutions by key stakeholders in the health sector. Many gaps can be identified through an exploration of the state of maternal and newborn health in Kenya:
Health-service delivery gaps
According to the 2014 Kenya Demographic and Health Survey (KDHS), only 61% live births occurring in Kenya are delivered in a health facility. 62% are assisted by a skilled provider and 53% of women receive a postnatal care checkup. Also, one in three newborns receives postnatal care from a doctor, nurse or midwife. With regards to vaccination coverage, only 79% of children (12-23 months) receive all basic vaccines. These statistics reveal the underlying gaps in access and utilization of essential maternity services by the public.
Many health facilities charge highly for various maternity services including emergency obstetric care. This makes the services less affordable and inconvenient resulting in an overall low uptake. Poor health infrastructural development marked by fewer health facilities in highly populated regions also causes accessibility problems which translate to poor maternal and child health outcomes. A number of facilities have few qualified staff with many unskilled attendants who put women and newborns at risk. All these service delivery factors collectively derail the efforts towards curbing maternal and newborn deaths in the country.
Environmental gaps
Expectant women and infants suffer the greatest brunt of ill-health in Kenya as a result of unfavourable environmental factors. The harsh environmental conditions in which infants are born make them vulnerable to malaria, diarrheal diseases, neonatal sepsis and respiratory infections. Informal settlement areas for instance are overcrowded with poor air quality as a result of poor waste disposal, scarcity in clean water supply and poor drainage. All these contribute to unhygienic conditions which make it hard to care adequately for newborns.
The situation is worsened by negative cultural beliefs and practices such as early marriages, emphasis on home deliveries and traditional cures. Data shows that some expectant women living around health facilities do not utilize Maternal and Newborn Health (MNH) services because of misleading cultural beliefs advocating for home-based care by elders; who in most cases are untrained.
Knowledge/Awareness gap
Despite the fact that majority of Kenyan women at least attain secondary education, most of them have little knowledge and awareness on many aspects of maternal and newborn health and overall reproductive health. This predisposes them to the risk of pregnancy-related complications and other sexual and reproductive health issues. The women may prove clueless when it comes to issues of family planning, breastfeeding, hygiene, proper nutrition, antenatal care, postnatal care, immunization among others. Knowledge plays a critical role in the maternal and newborn health outcomes of individuals and thus it remains a key factor at play amid the high mortality rates being witnessed.
MATERNAL/NEWBORN HEALTH AND THE VULNERABLE
Various categories of vulnerable women respond differently to their maternal and newborn health needs in Kenya. This is dependent on the prevailing conditions and the resilience of the affected individuals in coping with unforeseen events. A number of vulnerable groups and their typical responses in the utilization of maternal and newborn health is discussed below:
The poor and underprivileged
Poverty remains a great hindrance to good health and well-being particularly maternal and newborn health. Lack of finances to pay for vital health services leaves many women helpless when it comes to access and utilization of emergency obstetric care. For reasons of poverty and lack of essential newborn care commodities (baby clothes, soap, diapers etc.), majority of women forego hospital-based care. They feel stigmatized for showing up in health facilities with no basic newborn care items at the time of delivery. Also, poor women find it hard to access highly nutritive foodstuff during the pregnancy and postnatal period. This leaves them at risk of nutritional disorders and deficiencies which might have a reflection on the health and well-being of their newborns. There is an overall increased likelihood of low uptake of facility-based care among poor women in comparison to rich women.
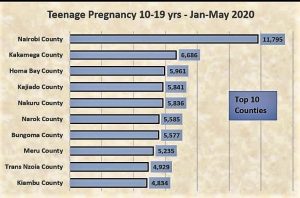
Teenage mothers
Teenage mothers are made vulnerable by the event of childbirth at a very young age which research confirms can be lethal and with lifelong consequences. In most cases, teens are clueless on almost all aspects of maternal and newborn health owing to their low literacy levels. They have limited knowledge and are just in the discovery face of life where sexual and reproductive health issues can be overwhelming to them. Typically, such young and vulnerable mothers shun from seeking medical care for reasons of fear of judgement and stigmatization. Some develop suicidal feelings especially those who become pregnant as a result of sexual abuse and molestation. They often miss their antenatal care appointments some even delivering their babies at home. The fear of bringing up a child single-handedly and possible termination of their education also causes anxiety for most of them. This reduces their morale and consistency in seeking maternal and newborn care in health facilities.
Slum dwellers
Informal settlement areas otherwise referred to as slums remain high risk areas when it comes to maternal and newborn health. These areas are characterized primarily by overcrowding, poor sanitation, poor housing conditions, inadequate fresh water supplies and high rates of social crimes all of which make it hard to offer or practice ideal maternal and newborn care. Slum dwellers due to congestion are mostly unemployed hence high dependency ratios remain endemic in such areas. That means that majorities cannot pay for essential maternal and newborn health services leave alone putting food on their tables. The areas have poor infrastructural statuses which make it hard, even impossible to access emergency obstetric care and other vital health services.
Typically, slum dwellers give preference to their survival (food and shelter) with little or no concern for their maternal and newborn well-being which is viewed as a secondary need and less important. They should however not be faulted for this because they are often left with no other options but to survive. It is because of this reason that health facilities continue to report few antenatal care contacts and hospital deliveries in such areas. Consequently, preventable maternal and newborn conditions such as pre-eclampsia, gestational diabetes, malaria, pneumonia and diarrhea remain endemic in the areas resulting in high mortality rates.
Mothers living with HIV/AIDS
HIV/AIDS has a great bearing on the maternal and newborn health statuses of women and children. The affected women need specialized care during pregnancy. This helps secure their newborns while at the same time safeguarding the health of the mother from opportunistic infections and childbirth-related complications. Prevention of mother to child transmission of the virus should be prioritized at all times. Women living with HIV/AIDS may fear to seek facility-based obstetric care for reasons of stigmatization or mistreatment. They may feel overwhelmed with the whole idea of prevention of mother to child transmission of the virus and thus need counselling and personalized user-friendly care. They may find it hard to consistently attend their antenatal care appointments, for this reason they need to be encouraged to adhere to ANC attendance recommendations. This can be achieved through incentivization and adoption of user friendly maternal health services.
Refugees and the homeless
Being homeless or in a refugee setting leaves many expectant women and newborns at risk for many preventable infections and possible death. Such individuals may lack almost all basic necessities including food, shelter, clothing and even security and are thus vulnerable. Refugees often have no access to quality maternal care and they may end up delivering their newborns without the assistance of health professionals. Antenatal care is absent for most of them. For the homeless, sleeping outside in the cold affects their health drastically resulting in infections which affect their pregnancy outcomes and the overall health of their newborns. Such individuals need assistance in seeking maternal care and finding comfortable housing facilities.
THE TOTO CARE BOX SOLUTION
Toto Care Box history
The Toto Care Box story began in 2012 in a little village called Marich in West Pokot, when Lucy Wambui Kaigutha (the founder) was working as a Public Health researcher collecting data on Integrated Management of Childhood Illnesses (IMCI). She had to conduct focus groups amongst women from this village. One mother stood out to her, she had five children, her fifth barely two weeks old and she had nothing. This woman stayed in Lucy’s mind long after she came back from West Pokot. She knew she needed to do something for the mother and her baby. One day she stumbled upon an article, “Why Finnish babies sleep in cardboard boxes” as she was browsing the internet and that was the inspiration for the Toto Care Box. In Finland, babies have been sleeping in cardboard boxes since 1939 after the Second World War as a government initiative to reduce maternal and infant mortality. Currently, Finland has the lowest maternal and infant mortality in the world. Lucy then decided to create the Toto Care Box tailored to suit the Kenyan needs and bring about similar outcomes. This would later be adopted for other high need African countries the aim being to save at least one million maternal and newborn lives in Africa by 2022.
How Toto Care Box promotes maternal and newborn health
Toto Care Box provides a simple but unified solution to the maternal and newborn mortality problem among vulnerable and underserved community members. This is achieved through a community-based integrated model bringing together health facilities, Community Health Volunteers (CHVs) and the target women. The main goal of the program is to increase access and uptake of quality life-saving maternal and newborn health services. The program is therefore important for a number of reasons; it provides a framework for achieving both the sustainable development goal and the Big 4 agenda related to maternal and newborn health. It is also critical in strengthening the health system through stimulating partnerships among the stakeholders in health. The program’s nature of working at the grassroots helps find more sustainable solutions which can be replicated in other high need areas in the country.
Toto Care Box addresses community maternal and newborn health needs in three major ways:
PROVISION – 18 maternal and newborn essentials are given to vulnerable women and newborns in order to prevent maternal and newborn deaths.
INCENTIVIZATION – women receive a Toto Care Box after attending at least four antenatal care visits and delivering in a health facility.
EDUCATION – women are educated on fundamentals of maternal and newborn care including danger signs during pregnancy and for the newborn, exclusive breastfeeding, proper hygiene, cord care and prevention of common newborn illnesses.

The program is guided by four core objectives all of which aim at reducing maternal and newborn deaths:
To incentivize women to attend at least four antenatal care visits.
These help in early detection and prevention of pregnancy-related complications such as hypertension and pregnancy diabetes both of which can dramatically affect the fetus. Early detection means regular monitoring and treatment.
To incentivize women to deliver in health facilities.
Facility deliveries by qualified birth attendants help reduce the chances of childbirth complications which often result in the death of a mother, her newborn or both.
To reduce the four major causes of newborn deaths (malaria, neo-natal sepsis, pneumonia and diarrheal diseases).
This is achieved by providing 18 low-cost, high-impact maternal and newborn essentials for the optimum survival of newborns.
To provide up-to-date maternal and neonatal information to women to ensure birth preparedness and effective childbearing.
This is done through mass education, Toto Care Box maternal and newborn care training as well as childbirth classes by Lamaze certified facilitators.
Solution targets
The Toto Care Box program prioritizes informal settlement areas of Kenya as well as other disaster prone and high need areas for its intervention. This is mainly because such areas are faced with serious problems when it comes to accessibility, affordability and acceptability of maternal and child health services and essentials. The areas are often characterized by poor living conditions and residents have high illiteracy levels and a diminished ability to make healthy choices. The primary beneficiaries are poor and underserved women and newborns but the program impact is generated at both household and community levels.
Impact
Currently, the Toto Care Box program works in 9 high need areas in Kenya and serves over 5000 underprivileged women and newborns. Through the program, a number of partnerships both local and global have been made aiming the betterment of maternal and newborn health outcomes for the poor. Also, the program has made great strides in impacting the lives of teen mothers and their newborns as well as mothers living with HIV/AIDS. Our hope is to give every newborn an equal and dignified start to life.
Call for support
We appeal to every interested persons, groups and organizations to support our highly potential cause (Toto Care Box) to reach out to other needy women. Support can be in form of financial assistance, donation of individual items (baby clothes, soap, diapers etc.), partnering in what we do, purchasing Toto Care Boxes for women or sharing our work with potential funders and donors. Feel free to reach out to us through the below contacts:
Website www.totocarebox.org
Email totocarebox@gmail.com
Phone +254701945110/ +254719313712
Conclusion
Evidence generated from the impact of the Toto Care Box program in Kenya reveals that maternal and newborn deaths can be prevented, reduced and even eradicated through simple but targeted interventions. Multi-factored and unified approaches need to be implemented especially in high need areas through synergistic partnerships by all the stakeholders in health. It is only through such client-centered methods that we will be able to secure our maternal and newborn health individually, communally, regionally, nationally and even continentally. Let us all strive to give each newborn a dignified and equal start to life.