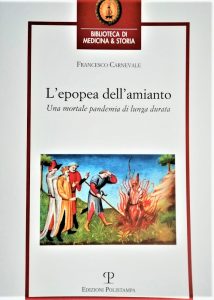
 Il presente testo è un ampio abstract del capitolo omonimo contenuto nel volume Francesco Carnevale, L’epopea dell’amianto. Una mortale pandemia di lunga durata, Polistampa, Firenze 2020, dove può essere consultata la bibliografia citata
Il presente testo è un ampio abstract del capitolo omonimo contenuto nel volume Francesco Carnevale, L’epopea dell’amianto. Una mortale pandemia di lunga durata, Polistampa, Firenze 2020, dove può essere consultata la bibliografia citata
di Francesco Carnevale
Medico del Lavoro Pubblico*
Il Rischio ed i Danni dell’Amianto nella Società, nei Media e nella Letteratura
Lavorazioni ed aziende fonti di esposizione
Il Novecento, in Italia come o di più che in altri paesi industrializzati, è trascorso con l’amianto come materiale ubiquitario e caratterizzandolo, grazie ad una sicura filiera di estrazione, importazione, produzione e commercializzazione, in particolare nel patrimonio edilizio, nella produzione energetica, di macchine industriali e di mezzi di trasporto; si deve dire che il Novecento è il secolo dell’amianto oltre che della silicosi.
Il più recente Rapporto Registri Nazionale dei Mesoteliomi (ReNaM), nella sezione documentazione, presenta, aggiornato, un Catalogo dell’uso di amianto nei comparti produttivi, macchinari e impianti; l’operazione è stata stimolata dall’interesse di assegnare al lavoratore colpito da mesotelioma una esposizione ad amianto. L’elenco è molto lungo e si può dire che comprende la quasi totalità delle più frequenti attività manuali, ma non solo queste, svolte da uomini e donne nel secolo scorso e ciò trova un corrispettivo nella mutazione nel tempo e nello spazio del genio epidemico degli effetti correlati con l’amianto.
Il più rilevante contributo delle asbestosi è fornito sino ad oltre metà del secolo dalle tessiture localizzate quasi esclusivamente nella provincia di Torino e dalla grande fabbrica di cemento amianto di Casale Monferrato; le asbestosi sono gravi ed i lavoratori colpiti generalmente non superano la “latenza” prevista per la manifestazione del mesotelioma, semmai alcuni si ammalano di tumore del polmone. Nel secondo dopoguerra si realizzano le “migliori” condizioni perché il mesotelioma si esprima con forza: l’estrema diffusione in quasi tutti i cicli lavorativi degli amianti ed anche di quelli considerati più pericolosi, la crocidolite e l’amosite, le relativamente più basse dosi di fibre assunte dagli esposti sia nei cicli tradizionali dove viene lavorato, sia in quelli dove l’amianto entra come materiale ausiliario; i lavoratori con o senza asbestosi hanno una più lunga aspettativa di vita che in passato e quindi un elevato rischio di ammalare di mesotelioma, non soltanto o forse non tanto nelle solite province piemontesi, ma anche o di più in ognuna delle aree portuali, nelle sedi dei nuovi insediamenti di fabbriche di cemento amianto, coinvolgendo anche i cittadini che abitano nelle vicinanze, e poi in quasi tutte le località del paese dove ci sono fabbriche che producono “beni e servizi”.
Si è parlato nei decenni più recenti di usi “impropri” dell’amianto, cioè di situazioni dove la fibra minerale assume un significato meno o per nulla correlato con i suoi noti vantaggi, specie in riferimento alla sicurezza. È difficile giudicare in generale, in maniera conclusiva, sulla “appropriatezza” di ognuno dei tanti impieghi dell’amianto se non dando valore assoluto, imprescindibile, alle conoscenze dei suoi effetti sulla salute e naturalmente al tipo di rischio subito. Non c’è dubbio che la “fiducia”, la “confidenza” del pubblico, dei consumatori, nei confronti dell’amianto e dei prodotti che li contengono sia stata forte, prolungata nel tempo, fomentata e poi mantenuta attivamente, anche con metodi fraudolenti; è altrettanto certo che, con il silenzio colpevole o l’avallo di chi, tra tecnici e medici ed amministratori pubblici, sapeva e non poteva non sapere, i produttori e chi traeva profitto dalla diffusione della fibra minerale hanno agito coscientemente conoscendo o almeno sospettando senza temerli i possibili effetti del proprio operato.
Il catalogo che qualcuno, senza ricorrere ad attenuanti di qualche genere, ha fatto degli usi “assurdi”, “impropri” dell’amianto potrebbe essere molto lungo e se ne propone un breve saggio. Piero Sampaolesi, protagonista del restauro di opere d’arte, con orgoglio illustra nel 1950 la sistemazione su pannelli di cemento amianto di affreschi staccati del Camposanto di Pisa ed in particolare il Trionfo della morte di Buonamico Buffalmacco e quello della Maledizione di Cam nelle Storie dell’Antico Testamento di Benozzo Gozzoli; le opere di recente sono state nuovamente restaurate e trasferite su nuovi supporti. La neve simulata con fiocchi di amianto è stata molto di moda, anche per evitare la lana, più facile ad incendiarsi, nella cinematografia americana ed in Europa; tra i tanti esempi si possono citare la celebre scena del Mago di Oz del 1939 di Victor Fleming ed anche il finale de La taverna dell’allegria del 1942 di Mark Sandrich o ancora le scene innevate in Quartiere dei Lillà del 1957 di René Clair. Fahrenheit 451 di Raymond Douglas Bradbury nel 1953 viene pubblicato in volume ed una tiratura di 200 copie ha una legatura in cartone amianto con qualche copia ancora presente nel mercato antiquario. Tra il 1952 ed il 1956 le sigarette Kent invadono il mercato munite di un esclusivo filtro Micronite ed un motto, “per la protezione migliore che potreste avere da qualsiasi sigaretta”; è stato accertato che il filtro è a base di crocidolite le cui fibre potevano essere inalate con il fumo. L’amianto e i suoi prodotti non hanno lasciato indifferenti architetti, designer ed artisti: Walter Adolph Gropius e Hans Scharoun hanno realizzato una enorme costruzione abitativa con cemento e amianto a Berlino tra il 1967 ed il 1969 e Le Corbousier una villa al mare nel Sud della Francia con tetto in cemento amianto; Norman Foster nel 1976 ha progettato una scuola a Liverpool tutta in cemento amianto colorato; Willy Guhl è famoso per la sua poltrona da spiaggia o da giardino del 1954 in cemento amianto. Alighiero Boetti ha creato nel 1966 la Catasta con tubi di cemento amianto oggi accolta nella Collezione del Castello di Rivoli; Enzo Cacciola ha realizzato negli anni ’70 dei quadri “materici” con cemento e asbesto su tela. Si può porre termine a questo catalogo di usi “impropri” ricordando che ancora alla fine degli ’80, fuori tempo massimo, la famosa Officina profumo-farmaceutica di Santa Maria Novella di Firenze ritaglia ed offre al pubblico dei dischetti in amianto da sistemare sul collo delle lampadine ad incandescenza per favorire così la diffusione di un composto aromatizzante per gli ambienti venduto assieme ai dischetti.
È indubbio tuttavia che in ogni paese ed anche in Italia e specie negli ultimi decenni si sono create delle situazioni che più di altre hanno sollecitato l’interesse collettivo anche perché oggetto di attenzione da parte dei media, della saggistica ed anche della letteratura. Si vuole far riferimento non tanto alla demonizzazione, alle volte fomentata strumentalmente, di manufatti in cemento amianto spesso di piccole dimensioni rispetto ai quali è conveniente adottare ragione e conoscenze scientifiche, bensì almeno a cinque vicende di “rilevanza nazionale. Il fatto che queste aziende, come tante altre, siano state oggetto di procedimenti giudiziari, con esiti i più vari, ha facilitato la ricostruzione delle relative esposizioni ad amianto e dei loro cicli lavorativi con testimonianze dirette di lavoratori e dirigenti aziendali raccolte in occasione di consulenze tecniche svolte per conto di alcuni Pubblici ministeri.
La Eternit di Casale Monferrato
Un italiano acquista il brevetto austriaco e fonda, nel 1906 Eternit Italia S.p.A. con stabilimento a Casale Monferrato da dove presto vengono immesse sul mercato, con enorme successo, lastre e tegole e dal 1928 tubi di varia foggia e quindi lastre ondulate, usate per tetti e capannoni tutto in cemento mescolato con amianto. Dagli anni ’30 e di più nel secondo dopoguerra con la “ricostruzione” l’industria del cemento amianto è sulla cresta dell’onda e nascono altre aziende Eternit e nuovi marchi come Fibronit. L’industria del cemento amianto è stata, e lo è ancora dove l’amianto viene ancora usato in molti paesi, la maggior utilizzatrice di amianto, arrivando a rappresentare l’85-90% dei suoi impieghi.
L’amianto giungeva, per ferrovia o per strada, nel reparto materie prime, in un sotterraneo, in sacchi di juta di circa 60 chili non proprio a tenuta che venivano aperti manualmente, senza alcuna protezione; l’amianto veniva messo a macinare nelle molazze che dovevano essere manutenute e pulite dagli stessi operai; l’amianto macinato veniva stoccato e quando necessario trasportato nel reparto impasto; negli ultimi 20 anni veniva inviato direttamente al reparto dove si facevano le miscele a secco con il cemento producendo un’enorme, continua nuvola di polvere tanto che, dicono gli operai, “Era impossibile distinguere i volti dei colleghi”; “Finito il turno ci si spolverava con l’aria compressa”. La miscela veniva spinta a pressione o fino alle macchine-lastre o fino alle macchine-tubi. Le lastre, una volta fatte e messe a riposo, venivano rifinite con operazioni manuali a secco e quindi polverose. La polvere si disperdeva abbondantemente all’esterno della fabbrica. I pezzi difettosi fino ai primi anni Sessanta venivano gettati in una discarica dove molti casalesi andavano per recuperarne alcuni; poi arriva il tempo del riciclo in un capannone senza mura, dove una ruspa le frantumava sollevando grandi quantità di polvere. I frammenti provenienti anche dagli altri stabilimenti del gruppo venivano portati a Casale e macinati. Gli operai dei settori più pericolosi avevano lo stipendio incrementato di circa ventimila lire rispetto agli altri, una “indennità di polvere” ma con questa e proprio per questa si “prendeva la polvere”.
Oltre che sindacalisti e lavoratori molti altri hanno scritto sul caso Casale Monferrato; la vicenda è stata sviscerata da medici ed epidemiologi ed ambientalisti, da giornalisti e giuristi, da sociologi, psicologi, da letterati, da scrittori di teatro, attori e filmaker, da storici, ed anche da ammalati di amianto e da loro familiari, colpiti terribilmente nel corpo e nello spirito. Si tratta di un corpus letterario unitario per tramandare e rievocare persone e fatti di enorme valenza sociale e scientifica. Eternit, dissolvenza in bianco è una opera che si occupa degli aspetti più importanti della storia dell’Eternit di Casale Monferrato; lo fa con una narrazione che ha come supporto il fumetto, il “fumetto-giornalismo” o meglio il “fumetto-storia”. La storia viene raccontata in 5 atti preceduti da un prologo e seguiti da un epilogo. Nel prologo, in una diecina di tavole, con didascalie essenziali scritte in prima persona e con solo due “nuvole” viene illustrato un “tipico caso” di diagnosi occasionale, dopo un lieve trauma toracico, di mesotelioma pleurico fatta nel 2004 in una donna giovane, piacente, attiva e sorridente ma residente a Casale. La storia “naturale” del “caso” rimane in sospeso, ma solo perché è considerata nota, a bassa sopravvivenza dopo la diagnosi, come ognuno degli oltre 50 mesoteliomi incidenti annualmente, di più ormai tra la popolazione generale di Casale, quella non esposta direttamente all’amianto all’interno della fabbrica. L’atto primo ha inizio nel 1957, quando in una modesta ma linda casa di Casale allietata da due pargoli giunge la notizia che il capo famiglia che aveva perso il precedente posto di lavoro viene assunto, “in pratica un’assicurazione a vita”, nella grande fabbrica dell’amianto; c’è grande serenità, si fa festa. Lo scenario cambia presto: preceduti da una tipica “entrata in fabbrica”, all’alba, di operai in bicicletta, siamo introdotti nei reparti di produzione al seguito di due nuovi operai, quello di prima, del 1957, ed anche, in una efficace intersezione cronologica, un altro che viene assunto nel 1974 e ciò in più episodi solo in apparenza indipendenti. I dialoghi e le immagini assieme ci rendono conto nel modo più completo di come venisse accertato e comunicato il rischio da polveri tra gli operai, praticamente solo all’interno del loro gruppo “omogeneo”; emerge così la “soggettività” operaia fatta di sintomi respiratori ingravescenti tra quelli con maggiore anzianità, l’individuazione motivata dei siti a maggior rischio con “grezze” ma essenziali valutazioni di ordine impiantistico e di igiene industriale dove le polveri, le nuvole di polvere, sono rese con dei segni forti, dei graffi minuti che suggeriscono il meccanismo con il quale esse aggrediranno le mucose, i polmoni, la pleura. Il secondo atto ha come titolo “la lotta dei lavoratori” e si apre con una morte, precoce, di un lavoratore affetto, ormai come tanti altri, da una grave affezione respiratoria; siamo nel 1979 e cominciamo a vedere delle immagini riferite al sindacato esterno, alla Camera del Lavoro di Casale, a dei protagonisti che della lotta all’amianto faranno la missione della propria vita sino ad oggi. In questa fase entrano in gioco: scioperi; il coinvolgimento delle varie strutture sindacali; l’acquisizione di conoscenze su tutti gli effetti dell’amianto compresi quelli cancerogeni; le vertenze per i miglioramenti delle condizioni di lavoro quando l’azienda assicurava di aver reso assolutamente salubre il lavoro in fabbrica tanto da smettere di pagare il premio assicurativo supplementare per l’asbestosi all’istituto assicuratore, l’Istituto Nazionale Assicurazione Infortuni sul Lavoro (INAIL), per la maggioranza dei lavoratori; la comparsa in scena per la prima volta della magistratura e le indagini peritali favorevoli per i lavoratori; la vertenza con l’INAIL con una manifestazione romana per il riconoscimento delle malattie professionali e di altri “diritti” previdenziali che si consideravano acquisiti; la preoccupazione per il ricatto della chiusura della fabbrica; l’evidenza del rapporto tra esposizione ad amianto e morte per tumori respiratori di compagni di lavoro. L’atto terzo è dedicato a “La lotta della citta” ed introduce, siamo nel 1982, un preoccupato sindaco di Casale che pensa a voce alta alle gravose decisioni da assumere anche in relazione ai dati inequivocabili provenienti dal Registro dei Tumori per il Piemonte e la Valle d’Aosta: “La mortalità da mesotelioma a Casale è 20 volte più elevata rispetto a quelle delle altre città”. Nel quarto atto, siamo nel 1988, a dominare la scena è la figura coraggiosa, eroica, severa della signora Romana Blasotti Pavesi che gravida di lutti familiari, “Mario, Piercarlo, Gianna, Paolo […]”, causati dall’amianto accetta di animare l’associazione di famigliari delle vittime per lottare, come è giusto le vittime facciano, per la bonifica del territorio, per stimolare la ricerca medica sui mesoteliomi e per chiedere giustizia, per evitare che altre vittime si aggiungano a quelle esistenti ed a quelle già destinate a soccombere. L’ultimo atto è quello della “bonifica” del sito aziendale richiesta con convinzione mediante popolate assemblee pubbliche e convincenti colloqui con le autorità dove emerge come un baratro l’assenza dell’azienda, l’unica responsabile dell’inquinamento. L’epilogo è un doveroso omaggio a Romana dolorosa ma implacabile nel chiedere che giustizia sia fatta.
Silvana Mossano, scrittrice ed assidua giornalista de La Stampa al processo Eternit che si celebra a Torino e profonda conoscitrice degli effetti sociali e medici dell’amianto anche per esperienza familiare, ha scritto un libro di grande valore letterario oltre che informativo. A giustificare tale affermazione basta richiamare il racconto Il Sospetto che occupa una delle quattro sezioni di cui si compone il volume; le altre sono: Donne nella polvere, testimonianze; Una storia lunga un secolo […] e non è finita, reportage; L’appello, lettera aperta. Vi si racconta, tra l’altro, una storia intima, rigorosa, ricca psicologicamente, di una madre, vedova, di Casale Monferrato che convive per un tempo interminabile col sospetto clinicamente consistente di avere un mesotelioma e quindi di dover lasciare in balia di sé stessa una figlia disabile.
Il giallista ed ingegnere elettronico bolognese Patrick Fogli, autore de Il tempo infranto, sulla strage alla stazione di Bologna, ha scritto un lungo e documentato noir che ha al centro l’amianto di Casale Monferrato. A svolgere delle indagini, ovviamente pericolose e contrastate da chi ne ha interesse, è una figlia giornalista che per il suo lavoro si era allontanata dalla città piemontese; la madre che aveva sempre abitato a Casale si ammala di mesotelioma, ma lei non aveva mai lavorato all’Eternit, aveva soltanto fatto l’insegnante. Le azioni, i viaggi e gli incontri della figlia vengono narrati parallelamente ad un diario, intimo, profondo, della malattia scritto in prima persona dalla madre.
Bruno Filippi è deceduto per mesotelioma in febbraio, la sua Cronaca della dipartita che nel titolo completo del suo libro comprende l’espressione il Morbo di Casale e la parola credente annuncia con fedeltà ciò che effettivamente si troverà diffusamente nel testo. Una peste o un colera endemico e apparentemente insanabile che affligge, come un castigo, un territorio abitato da gente industriosa che non merita questa pena e poi il racconto delle “difficoltà” causate dal mesotelioma che accompagna sino alla morte un cristiano devoto, onesto, attivo, un giusto che, senza rassegnazione e senza rabbia, riesce ad esprimere sino alla fine amore per la famiglia, per gli amici, per quelli accomunati con lui dalla sventura, per Dio; gli danno forza le attenzioni dei suoi cari, la preghiera e la giustizia divina sostenute dalla fede e quindi dalla vita che senza dubbio alcuno sino alla fine deve essere sempre rispettata e vissuta assegnando così un senso al dolore ed alla morte.
Il 6 aprile 2009 inizia presso il Tribunale di Torino il processo contro uno dei due fratelli Schmidheiny, ex presidenti del consiglio di amministrazione dell’Eternit AG, ed il barone belga Jean Louis De Cartier de Marchienne; del 2011 è il rifiuto dell’offerta di una contropartita economica al comune di Casale per abbandonare la costituzione di parte civile al processo; il 13 Febbraio 2012 il tribunale di Torino emette una sentenza storica, condannando in primo grado gli imputati a 16 anni di reclusione “per disastro ambientale provocato dall’amianto”, e obbligandoli al risarcimento di circa 3000 parti civili oltre al pagamento delle spese giudiziarie; sentenza sostanzialmente confermata in appello 2013 e poi vanificata in Cassazione nel 2014 per intervenuta “prescrizione del reato”; nel 2015 partono nuovi processi decentrati in relazione all’“omicidio colposo” di alcuni singoli lavoratori, l’Eternit bis.
Dalla metà degli anni ’80 in poi numerosi studi epidemiologici a cominciare da quello sui lavoratori seguito da quello sulle loro mogli e poi sulla popolazione generale, percorrendo un processo di assidua sorveglianza epidemiologica, portano alla conclusione che la mortalità per neoplasie pleuropolmonari e peritoneali nell’area di Casale è straordinaria, nettamente superiore all’atteso; a portare il grosso fardello di morte per mesotelioma sono prima gli operai dell’Eternit e più di recente i cittadini di Casale con circa 50 casi all’anno. I dati per il periodo 1990-2014 indicano un andamento temporale non più in crescita che appare invece stabilizzato o anche in decremento.
La Società Italiana Amianto di Grugliasco
In Grigio è il colore della polvere è una giovanissima operaia, Germana, immigrata degli anni ’60, con tutti i suoi sentimenti, le sue aspirazioni, che ci introduce all’interno della famigerata Società Italiana Amianto (SIA) di Grugliasco. Il racconto continua seguendo la sua famiglia. Poi sono illustrate le storie personali di Raffaele, di Teresa, di Luigi e Rosina, di Lina, Rita e Maria e di Gina e di tanti altri arrivati dalla Calabria, dal Veneto, dalla Sicilia per vivere nella ed attorno alla fabbrica grigia che tuttavia all’ingresso sfoggiava roseti ed un laghetto. L’autore dell’inchiesta, Luca Ponzi, adotta la seguente epigrafe “I personaggi di questo libro sono realmente esistiti, i fatti narrati sono davvero accaduti. Purtroppo”. Nel resoconto incombente è la fabbrica, poi entrano in campo la città, un processo giudiziario, dei consulenti tecnici, dei mediatori culturali, dei provvidenziali “facilitatori” che man mano diventano comprimari. Opportunamente il libro si conclude con un capitolo che parla del “futuro” che non mira soltanto alla fine di una vertenza giudiziaria bensì ad un ventaglio di iniziative coordinate in un centro creato ad hoc da istituzioni avvedute che lavorano alacremente per la bonifica del territorio e, per quanto possibile, per la prevenzione secondaria, la diagnosi precoce e per quella così detta terziaria, la “riabilitazione”.
Questo volume rappresenta la giusta continuazione o comunque è complementare di un precedente, particolarmente toccante, reportage, Digerire l’amianto composto originariamente da Chiara Sasso nel 1990 per iniziativa del Comune di Grugliasco. Il risultato è un racconto di un coro composto da individui, da donne operaie riunite in varie occasioni dall’autrice e capaci di riferire e commentare anche argutamente ricordi, esperienze, aspirazioni; il leitmotiv è quello di un lavoro inteso come una sofferenza necessaria, all’inizio senza escludere la possibilità di “scamparla”, alla fine con legittime rivendicazioni, ma non con particolare astio, nei confronti di padroni, INAIL, sindacati, partiti, magistrati, sindaco e stato.
Le origini della SIA sono ottocentesche con produzione principale di filati in amianto per fabbricare stoppini per l’illuminazione pubblica a gas. Nel 1907 viene fondata la Società Anonima Italo-Russa per l’Amianto (SIR) perchè l’amianto viene dagli Urali; la produzione si amplia ed oltre ai manufatti per guarnizioni vengono immessi sul mercato filati, tessuti e nastri e, tra le due guerre, guarnizioni d’attrito per freni; nel 1951 la SIR cambia intestazione in SIA S.p.A.. Alla metà degli anni ’60, in un periodo di grande espansione, conta circa 700 dipendenti tra operai ed impiegati e produce in quattro stabilimenti. Il declino è della metà degli anni ’70, causato da una riduzione della domanda dei prodotti contenenti amianto e dalla rinuncia a nuovi investimenti; del 1982 è la comunicazione ai sindacati della volontà di liquidare l’azienda, ma c’è il tempo per il cambio di proprietà e di ragione sociale e SIA acquista una lettera diventando SIA A, dove la seconda A sta per “Alternativi” (all’amianto). La chiusura definitiva è del 1986.
La produzione della SIA negli anni più recenti si svolgeva su sei linee di produzione: filati, tessuti, corde, sirite, gommati, carta e cartone. Semilavorati di varia foggia potevano essere spalmati con elastomeri naturali o sintetici per impermeabilizzarli e poi venivano lavorati, tagliati, calandrati, stampati.
Gli studi sulle malattie dei lavoratori della SIA non sono abbondanti. Una prima indagine sulla mortalità per tutte le cause e poi quella correlata con l’amianto, lunga e difficile, è stata svolta da Benedetto Terracini e da suoi allievi a partire dal 1975 in un ambito giudiziario; i risultati sono stati utilizzati per avviare il procedimento di omicidio colposo per il decesso di 32 lavoratori conclusosi con la condanna di alcuni dirigenti dell’azienda nel 1996 e poi, di nuovo per altri 23 operai morti, nel 2004. I dati completi dell’indagine non risulta siano stati pubblicati su riviste. Del 2012 è uno studio di Maria Cacciabue, Guia Benedetto, Francesca Filippi che utilizzando i libri paga della ditta ed il sistema informatico INAIL, individua 776 donne sul totale di 1215 lavoratori assunti dalla SIA tra il 1960 ed il 1978. Considerando il luogo di nascita risulta che 90 lavoratrici provenivano dal Piemonte, in particolare 46 dal comune di Grugliasco, Collegno e limitrofi; delle 686 originarie di altre regioni, 245 sono nate in Sicilia, 147 in Veneto, 60 in Puglia, 40 in Campania, 30 in Calabria, 19 in Sardegna, 18 in Emilia Romagna, tutte provenienti dalla provincia di Ferrara; delle nate in Sicilia, 35 provengono dalla provincia di Caltanissetta; tra le assunte sono stati rilevati 123 gruppi parentali e 48 riassunzioni. Dalla verifica dello stato in vita di tutte le lavoratrici risultano 99 decessi, in 43 casi correlati causalmente all’esposizione ad amianto, in particolare si sono verificati 20 decessi per neoplasie mesoteliali ed 8 per neoplasia polmonare. Tra le donne decedute, 25 risultano avere una rendita INAIL per patologie asbesto correlate; di queste 16 sono decedute per patologia neoplastica da amianto con 12 casi di neoplasia da amianto non indennizzati, manifestatasi nella maggior parte negli anni settanta-ottanta, quando generalmente quella patologia non veniva riconosciuta dall’istituto assicuratore in carenza della diagnosi di asbestosi; 113 lavoratrici viventi avevano una rendita INAIL per malattia professionale. Dai dati forniti risalta un fenomeno molto importante, quella forma di autotutela adottata dalle lavoratrici riducendo la dose di amianto inalato abbandonando prima possibile quella fabbrica.
Da tempo erano disponibili le informazioni riguardanti la coorte dei lavoratori della SIA ed il più recente studio di mortalità con follow-up al 2013 di 1977 lavoratori di cui 1083 donne che vi hanno lavorato tra il 1946 ed il 1984 è capace di illustrare un quadro veramente impressionante: tra le 1019 morti osservate si registrano 60 mesoteliomi della pleura dei quali 36 in donne; 48 mesoteliomi del peritoneo dei quali 36 in donne; 143 tumori del polmone dei quali 42 in donne; 15 tumori dell’ovaio.
Il registro nazionale dei mesoteliomi per quanto riguarda il comparto tessitura di amianto riporta complessivamente, per il periodo 1993-2015, 129 casi di mesoteliomi dei quali 95 in donne; le regioni con maggiore peso della categoria sono Piemonte con 92 casi e Lombardia con 26.
L’Amianto di Balangero
Sorge il Monte San Vittore al confine tra i Comuni piemontesi di Corio e Balangero. E’ qui che nei primi anni del Novecento vengono scoperte delle vene di fibra minerale con sicuro valore economico. Nel 1918 viene costituita la Società Anonima Cave San Vittore che acquisisce terreni per installare impianti importanti dal Canada, crea strutture per il trasporto del materiale, cerca di assicurarsi la committenza della Eternit di Casale Monferrato; una discreta produzione, ancora con un notevole disavanzo economico, inizia nel 1921; l’amianto di Balangero avrà una grande visibilità partecipando come protagonista alla Mostra del minerale di Roma ed alla Mostra dell’autarchia di Torino, tenutesi entrambe nel 1940.
La Società decide di svolgere ricerche per estrarre il nichel dalla cava di Balangero e Primo Levi (1919-1987), allora neolaureato, nel novembre del 1941, recandosi in incognito sul monte San Vittore, compie ricerche e prove di estrazione del nichel dalla roccia di serpentino, ci rimarrà sino al giugno 1942. Lo scrittore torinese narrerà con un certo entusiasmo questa sua breve esperienza nel capitolo Nichel della raccolta di racconti Il Sistema periodico soffermandosi con indubbi effetti letterari su aspetti del paesaggio, del ciclo lavorativo, della polvere imperante e su scene di costume capaci di connotare meglio chi nella cava di Balangero spende la propria vita.
Sotto la Repubblica di Salò e l’occupazione nazista l’azienda viene posta sotto sorveglianza di un “Incaricato per l’amianto”, che impartisce disposizioni sulla produzione, vendita e, principalmente, esportazione in Germania del minerale. Il bilancio economico del primo dopoguerra è in grave sofferenza ma nel 1950 la Società Cave San Vittore passa dall’IRI al gruppo Manifatture Colombo ed alla multinazionale Eternit e, nel 1951, viene costituita l’Amiantifera di Balangero S. p. A. arrivando negli anni successivi al massimo della produzione e dei profitti ma anche suscitando forti conflitti sindacali.
Tra i documenti della cava di Balangero conservati presso l’Archivio di stato di Torino è presente un dossier contenente la rassegna stampa sugli scioperi operai degli anni ’50; è stato rinvenuto tra gli altri un articolo di Franco Bertone, Scavano la montagna e invecchiano nella polvere pubblicato da la Battaglia Democratica di Torino del 24 ottobre1949. Di domenica 28 Febbraio 1954 è un pezzo illustrato da due disegni tanto lineari quanto espressivi di Mino Rosso; iI titolo, probabilmente non redazionale, è La fabbrica nella montagna, la firma è quella di Italo Calvino, un prezioso “racconto breve”. Calvino costruisce una scenografia, il grigio, la polvere, i boschi, la montagna, i gradoni, i pozzi sanguinolenti, la fabbrica ma scrive nel contempo una sceneggiatura intensa, di una vicenda epica interpretata da personaggi autentici, che svolgono in pieno il proprio ruolo; gli operai del turno da coro informe si trasformano in protagonisti della scena che è e si mostra in tutta la sua drammaticità.
Nel 1957 l’Amiantifera di Balangero ha circa trecento dipendenti, raggiunge punte di produzione di centocinquanta tonnellate al giorno ed il bilancio è in attivo. Nei primi anni ’50 viene sostituito il sistema di coltivazione a glory hole con quello a semi-anfiteatro con gradoni sovrapposti di circa quattordici metri; si abbandonano gradualmente le cariche esplosive per l’abbattimento della roccia per usare degli escavatori tipo ripper; i famosi trenini “Gibuti” lasciano il posto a nastri trasportatori e dumper. Viene immesso sul mercato come filler anche il materiale povero, con basso tenore di amianto, finisce nei settori lavorativi più vari da quello dei conglomerati bituminosi alla costruzione delle strade ed anche di quelle ferrate diffondendo il rischio da amianto tra una moltitudine di lavoratori più spesso ignari. Una maggiore automazione degli impianti, a cavallo degli anni Sessanta e Settanta, consente una maggiore produzione ed anche una riduzione della polverosità nelle varie postazioni di lavoro e nell’ambiente generale; l’insaccamento della fibra viene fatta dalle macchine ed i sacchi di carta e poi di materiale plastico sostituiscono quelli di juta. Inoltre, la pulitura delle macchine, fino ad allora eseguita mediante soffi di aria compressa, viene ora effettuata attraverso un sistema centralizzato di aspirazione con filtro che diminuisce la dispersione delle polveri; viene reso meno invadente ed inquinante l’accantonamento dei materiali di scarto dell’attività estrattiva.
Il paternalismo viene praticato volentieri all’Amiantifera ed alcuni lavoratori la ricordano con una certa nostalgia; al quindicesimo anno di lavoro in cava viene corrisposto un premio di fedeltà, un orologio con medaglia incastonata su serpentino, regalie in denaro, il ricco festeggiamento annuale, il 4 dicembre di S. Barbara, frequentato anche da ex partigiani, asili nido, palestre, sale di riunioni nei paesi del territorio.
L’era espansiva dell’Amiantifera di Balangero S.p.A. si conclude nel 1983; è l’inizio della fine che culmina nel 1990 con la dichiarazione di fallimento. Dal dicembre 1989 i lavoratori della cava rimangono senza stipendio ed il Comune di Corio in attesa della “Cassa integrazione guadagni” rende possibile, assumendosi l’onere degli interessi, la corresponsione di una quota della liquidazione. Di questa fase della cava di Balangero tratta il libro scritto con verve e passato sotto silenzio anche nei circoli più specializzati sul tema dell’amianto da Enzo Biagioni, un tecnico di origine toscana. Una spiegazione di questo silenzio potrebbe essere riconosciuta nel fatto che l’autore si muove in controcorrente; benché il racconto di storia vissuta abbia al centro le difficoltà insorte nell’applicazione delle norme a favore dei lavoratori collegate con la decisione della “singolare” dismissione della cava di amianto, l’autore dichiara in maniera abbastanza esplicita il suo disappunto e quello di tanti altri, lavoratori ed abitanti della valle, sulla chiusura o almeno sulle modalità con le quali la chiusura della cava è stata attuata. Il libro si fa comunque apprezzare per alcune testimonianze sulla vita che si svolgeva nei decenni passati nella cava; attenzione e sospetti vengono dedicati poi, purtroppo con pochi dati solidi, all’ultima proprietà di Balangero, portatrice di interessi, anche per conto di politici, per affari poco chiari in riferimento a rifiuti e discariche da sfruttare; si parla di tangenti a non finire, di un complotto della FIAT che aveva la necessità di utilizzare come discarica “questo buco unico in Europa” e della Montedison che aveva introdotto sul mercato il retiflex, un materiale prodotto sinteticamente che nel fibrocemento poteva sostituire l’amianto.
Già nel 1992, con la legge di dismissione dell’amianto lo stato, nonostante il sito non fosse di proprietà o gestione pubblica preventivava, con rituale “riserva di rivalsa”, complessivamente trenta miliardi di lire per la bonifica della cava San Vittore; poi una legge giustamente considera il sito da bonificare di interesse nazionale. Oltre allo smantellamento delle strutture, sono previsti lavori di sistemazione idrogeologica e di messa in sicurezza tramite l’impiego di tecniche di ingegneria naturalistica della zona di estrazione e delle discariche ubicate in gran parte nel territorio di Corio. Gli interventi iniziati nel 1995, proseguiranno per un tempo indeterminato con costi sempre in crescita; un obiettivo è anche quello di realizzare un ecomuseo ed estesi campi fotovoltaici.
Gli effetti sulla salute dei minatori, sono presi in esame nella indagine ampia ed approfondita pubblicata nel 1972 e si tratta di uno dei primi se non del primo studio di coorte svolto in Italia. La coorte è composta da 1098 lavoratori, solo cinque sono donne, con “rischio di asbestosi”, dei quali 242 al lavoro al 31 marzo 1970 con un’età media non elevata; di 998 si sono ottenute informazioni e di questi 270 risultano morti. Una mortalità più elevata non viene rilevata tra i lavoratori considerati a maggior rischio che appaiono, con una sorta di “effetto lavoratore sano”, “selezionati”; le cause di morte più frequenti appaiono essere legate alle condizioni socio economiche del territorio, cardio vascolari, traumatiche, anche diverse dagli infortuni sul lavoro, respiratorie, dell’apparato digerente; 6 sono i deceduti per tumore polmonare, tra i quali solo uno non fumatore, e nessun per mesotelioma; incidenza questa valutata come sovrapponibile a quella degli abitanti di Balangero e Corio che porta gli autori ad escludere per i minatori, a differenza che in altre analoghe straniere, una correlazione tra amianto e tumori. Questa vulgata viene tramandata per molto tempo e nella sostanza accolta e sostenuta da alcuni lavoratori, da amministratori dei comuni interessati alla cava e non contrastata, anzi implicitamente avallata dai medici dell’Istituto di Medicina del Lavoro di Torino. Chiarezza verrà fatta grazie al Registro dei Mesoteliomi Piemontese che consentirà di illustrare con i criteri scientifici del caso i 27 mesoteliomi diagnosticati tra il 1980 ed il 2007, 14 tra quanti sono stati attivi nella cava e 13 tra esposti attraverso diverse modalità̀ all’amianto di Balangero. Un lavoro del 2008 pubblicato elaborando i dati del Registro e lo studio di coorte del 2019 oltre che rendere ragione della dimensione dell’impatto patologico, più vicino alla realtà, svolto dallo sfruttamento della cava, coadiuva con decisione alla demolizione della teoria che vuole il crisotilo non inquinato dall’anfibolo tremolite, come è quello di Balangero, privo di effetti cancerogeni per l’uomo.
Molti lavoratori italiani hanno vissuto la terribile esperienza lavorativa in una miniera di crocidolite australiana, Filippo La Torre racconta in buona forma letteraria di un ventenne palermitano che va in frontiera, nella British Columbia, raggiunge il fratello maggiore e lavora in una cava di amianto crisotilo. Salvatore, “Sal”, intraprendente ed aitante, tipica espressione dell’“effetto lavoratore sano”, opera in quella realtà, a 2.000 metri di altezza, in un clima estremo con inverni a -40°C e comunque dalla bellezza stupefacente in due diversi periodi, dal 1962 al 1968 e dal 1978 al 1980. “Sal” raccoglie ed organizza in maniera quasi ossessiva i ricordi e le immagini della sua vita di minatore che arrivano così nelle mani del figlio Filippo. Il risultato molto apprezzabile è pur sempre una fiction ma molto documentata anche dal punto di vista tecnico che soddisfa e può anche entusiasmare chi vuol sentire parlare dell’emigrazione italiana, della socialità, dell’amicizia e della solidarietà, della multietnicità, di sesso, alcool e droga, delle bellezze naturali, di caccia e di pesca ed anche di amianto. Seguendo il protagonista nello svolgimento delle varie mansioni, dallo sguattero in cucina allo specialista delle esplosioni, apprendiamo tutto quanto succede in una cava ed in un villaggio minerario; le singole fasi lavorative sono descritte con buona precisione tecnica, arricchite dalle “reazioni” e dalla organizzazione informale, compresi molti comportamenti contrari alla sicurezza, messe in atto dagli operatori.
L’amianto dei treni
Negli anni ’40 del Novecento amianto viene impiegato per la coibentazione di parti delle locomotive a vapore, tubazioni della caldaia e guarnizioni di tenuta, in alcuni casi della stessa caldaia. Nelle carrozze amianto crisotilo in forma di nastri, corde e cartoni può essere presente nei mezzi di accoppiamento vapore cioè nelle condotte di trasferimento del vapore dalla caldaia o carro riscaldatore alla carrozza, nelle tubazioni di trasporto del vapore ubicate nel sottocassa e, all’interno della carrozza, nelle aree di emissione del calore, dette scaldiglie ubicate sotto i sedili dei passeggeri e nel retroschienale di alcuni tipi di carrozze.
Dall’inizio degli anni 50 viene imposto alle ditte di costruzione di nuovi rotabili che le lamiere della scocca siano spruzzate con amianto e, almeno per alcuni anni, prevalentemente crocidolite e ciò anche sul soffitto della cabina di guida di alcuni modelli di locomotori elettrici; l’impiego della crocidolite sembra cessare, ma non immediatamente, negli anni successivi al 1971 quando una ditta incaricata della coibentazione, la Davidson, chiede il permesso alla Ferrovie di Stato di non utilizzarla perché di difficile reperimento sul mercato.
Dalla fine degli anni ’50, così come facevano la maggioranza delle aziende ferroviarie dei vari paesi, ma anche come conseguenza di un incidente che aveva comportato l’incendio di carrozze motrici ed il decesso di passeggeri, le Ferrovie dello stato (FS) decidono di coibentare con amianto spruzzato anche le carrozze già circolanti, gli elettrotreni adibiti al trasporto passeggeri e le cabine di guida dei locomotori. Queste operazioni di coibentazione avvengono anche nelle officine ferroviarie e sono affidate in convenzione di appalto a ditte private; un elettrotreno risulterà coibentato con circa una tonnellata di amianto, una carrozza con una quantità che varia da circa mezza ad una tonnellata per i vagoni letto, postali e bagagliai. Da più fonti risulta che la coibentazione venivano effettuate senza particolari precauzioni; a partire dal 1968 in ambiente appartato o all’aperto nel parco rotabili e, nell’ultimo periodo, in giornate non lavorative. Come in altri comparti lavorativi anche in quello ferroviario vengono considerati esposti e quindi assicurati, soltanto i lavoratori che utilizzano la fibra minerale in maniera esclusiva o prevalente, come i coibentatori che in genere non sono dipendenti dell’azienda che li utilizza “in appalto”; tutti gli altri lavoratori, falegnami, pannellisti e lamieristi, verniciatori, elettricisti, tappezzieri, manovali, che lavorano “in presenza” di amianto, nelle vicinanze di coloro che lo utilizzavano come materia prima, o che lo utilizzano in maniera non continuativa non vengono considerati esposti e quindi, e il consenso dell’ente assicuratore, l’INAIL, non sono coperti dal rischio amianto e per loro non viene pagato il premio supplementare per l’asbestosi e ciò con il duplice effetto di ridurre il costo del lavoro e di evitare di adottare le misure tecniche di prevenzione e la sorveglianza sanitaria del caso.
Dalla metà degli anni ’70 fino agli inizi degli anni ’80 tutti gli impianti delle FS intervengono su rotabili precedentemente coibentati con amianto spruzzato, oltre che continuare ad utilizzare manufatti contenenti amianto. In particolare nelle Officine Grandi Riparazioni (OGR) l’occasione dell’esposizione degli addetti ad alcune mansioni quali tappezziere, elettricista, falegname, meccanico, lamierista-pannelista e verniciatore varia per frequenza ed intensità in relazione alla tipologia di rotabile; infatti la quantità di amianto nei rotabili risulta essere presente in maniera non uniforme. A partire dalla metà degli anni ’70 cessano da parte delle FS gli ordinativi di carrozze coibentate con amianto, mentre le ultime consegne dalle aziende costruttrici sono del 1978.
Nei primi anni ’80 nell’azienda delle FS viene messo in moto, stimolato anche dai sindacati dei lavoratori del settore, specie in alcune realtà produttive, a Torino ed a Bologna, un processo comprensivo di “fuoriuscita dall’amianto” e di gestione tecnica delle varie fasi attuative: effettuare la decoibentazione totale dei veicoli coibentati con amianto costruendo condizioni idonee per la sua rimozione e per le attività lavorative che pur devono essere svolte in presenza di amianto sulla base di norme tecniche diramate nel 1983 integrate successivamente, concordate con la dirigenza delle organizzazioni sindacali di categoria. Ciò, che in altri paesi era iniziato molto tempo prima, in Gran Bretagna almeno dal 1967, viene realizzato con un certo impegno finanziario entro il primo quinquennio degli anni ’80 e conduce ad una diversa organizzazione del lavoro ed alla ristrutturazione o costruzione di nuovi ambienti di lavoro. Il piano decennale prevede di avvalersi di dieci OGR attrezzate e dell’intervento di sei ditte esterne alle FS per effettuare la decoibentazione di 516 locomotive elettriche, 1002 mezzi leggeri elettrici, 271 mezzi leggeri termici, 4044 carrozze.
Del 1983 è la decisione, già nell’aria da qualche tempo, fortemente voluta dalle organizzazioni sindacali delle FS, di far effettuare specialmente all’industria privata la decoibentazione dei veicoli ferroviari. C’è la rincorsa all’“affare” nel quale si buttano a capofitto anche imprenditori improvvisati nella materia.
Verso la fine del 1983, 348 lavoratori delle FS denunciano al pretore un rischio elevato da amianto per la salute all’interno delle OGR di Porta al Prato di Firenze e nelle cabine di guida di alcuni mezzi di trazione. L’intervento del pretore, con i poteri più estesi dell’epoca si concretizza nel 1988 con l’invio di comunicazioni giudiziarie ad alcuni dirigenti FS e con la chiusura dell’Isochimica di Avellino visitata dai tecnici della Unità Sanitaria Locale (USL) congiuntamente con il pretore fiorentino; infatti da quella azienda provenivano veicoli scoibentati in maniera incompleta sui quali dovevano poi intervenire i lavoratori di Porta al Prato. La chiusura dell’Isochimica si impone per motivo di giustizia, per interrompere il perpetuarsi del reato. Al magistrato fiorentino pervengono altre denunce di situazioni di rischio da parte di lavoratori di altre strutture FS del paese; con la stessa logica giuridica viene svolto, su richiesta dei lavoratori, un sopralluogo ed il successivo sequestro da parte del medesimo pretore delle OGR di S. Maria la Bruna.
Le insufficienze dei provvedimenti applicati dall’azienda nelle OGR di Firenze, segnalate dagli operatori delle USL, trovano validazione da parte di una Commissione appositamente nominata da FS, composta da esperti del settore in ambito nazionale, per lo studio del problema amianto. Viene emanata una nuova Circolare, nel 1989, che precisa, aggiornandole e migliorandole, le procedure di lavoro in presenza di amianto.
Nel 1999, secondo i dati forniti da FS, il “parco rotabili” con amianto spruzzato o con materiali contenenti amianto ed anche quelli accantonati in attesa di bonifica e successiva rottamazione risultano sottoposti ad un censimento e ad un programma di controllo interessando circa 450 rotabili circolanti con coibentazione in amianto, circa 3300 rotabili circolanti decoibentati prima del 1990, circa 2800 rotabili accantonati in attesa di bonifica per successiva demolizione, circa 1400 carri con possibile presenza di amianto nelle condotte.
La segnalazione di un aumento del rischio di mesoteliomi nel settore ferroviario in Italia ha inizio con lo studio commissionato da FS ad un gruppo di “consulenti” sugli addetti dell’OGR di Foligno pubblicato nel 1986. I risultati dell’ampia indagine con la partecipazione di molti operatori del Sistema sanitario nazionale e di alcune Università vengono resi noti nel 1990 e nel 1991 rilevando una dimensione non sospettata della gravità e diffusione del rischio. L’ultimo aggiornamento della coorte degli operai maschi della Breda di Pistoia, produttrice di carrozze ferroviarie, effettuato dal 01/01/1960 al 31/12/2010 evidenzia 22 tumori della pleura e 2 del peritoneo e retroperitoneo. Lo studio epidemiologico di mortalità nella coorte di lavoratori dipendenti FS assegnati all’OGR di Bologna con un periodo di follow-up che va dal 01/01/1960 al 31/12/2014 ha mostrato 107 mesoteliomi. Uno di questi “casi” è quella del marito di una grande donna che racconta la storia del marito “che ha cercato di combattere fino alla fine ‘il killer invisibile’ […] l’Amianto”; è un diario suo, del marito e della sua famiglia inesorabile, clinico e spirituale dove si narra il percorso di un malato con tutte le sue veritiere espressioni psico-fisiche che riesce a mantenere sino alla fine la dignità di uomo, di cittadino, di lavoratore, di padre e di marito. Almeno tre punti sono risultati e permangono prepotenti nella vicenda: il figlio diciassettenne che vuole rimuovere il problema di suo padre, che non vuole sentirne parlare per quanto sta male; la sintonia tra la moglie e l’assistenza pubblica fatta anche questa di persone vere nel mettere in atto il “sostegno e l’accompagnamento”; e poi un desiderio che non in modo sorprendente guida l’autrice nella scrittura dell’ultima parte del diario.
Il Registro Nazionale dei Mesoteliomi nel suo sesto rapporto nella categoria “Rotabili ferroviari (costruzione e riparazione)” riporta, per il periodo 1993-2015, complessivamente 619 mesoteliomi; le regioni con maggiore peso della categoria sono Emilia-Romagna con 168 segnalazioni, Veneto 112, Toscana 89. Le mansioni maggiormente coinvolte sono saldatori e tagliatori a fiamma, montatori di carpenteria metallica, installatori e riparatori di apparati elettromeccanici, ebanisti, falegnami e operatori artigianali di macchine per la lavorazione del legno.
L’amianto delle navi
Negli scafi dei natanti, sia civili che militari, ed anche nei motori è stato da sempre fatto largo uso di anfiboli e crisotilo friabili, materassi, tessuti di foggia varia, e di materiali più o meno compatti, intonaco in cemento rinforzato con fibra di amianto, cartone di amianto forato, tela in amianto verniciata, marinite laminata; le finalità erano quelle abituali per le quali la fibra minerale era invocata anzi resa obbligatoria da norme tecniche e dalle esperienze belliche delle battaglie navali: protezione contro il “fuoco nemico”, fonoassorbimento, antirombo, isolamento termico, anticondensa; in più nei cantieri navali venivano utilizzati teli amiantiferi per motivi tecnici, in occasione di saldature, e per proteggere i saldatori. Spesso l’esposizione ad amianto nella nave-fabbrica si associava per la maggior parte dei lavoratori alla esposizione ad altri fattori rischio, fumi, gas, vapori, alcuni dei quali dotati di sicura cancerogenicità.
Tra Otto e Novecento inizia la coibentazione degli apparati motori delle navi a vapore e poi quella dei motori a turbina e dei motori a scoppio; indicativamente, a parità di tonnellaggio, l’apparato motore di una motonave aveva circa 7 tonnellate di materiale coibente e quello di una turbonave circa 30 tonnellate. Caldaie, camini, tubazioni, valvole, ecc. sono ricoperti, con criteri codificati, di manufatti di amianto; quindi nell’allestimento e nell’addobbo dei natanti, degli alloggi e delle cabine, entrano a far parte molti materiali prefabbricati e non con impasti di amianto con altre sostanze in forma di paratie tagliafuoco, pavimenti, ecc. I pannelli di amianto usati per l’allestimento di un grosso transatlantico ricoprono una superficie totale da 50.000 a 120.000 metri quadrati per un peso complessivo variabile da 500 a 1500 tonnellate. Negli anni ’30 fa la sua comparsa e poi entra massicciamente l’applicazione dell’amianto a spruzzo, miscelato con acqua e collanti, su paratie, soffitti e strutture varie. Spesso l’uso di amianto procede parallelamente con l’impiego di altri materiali coibenti “sostitutivi”, lane di vetro e di roccia disponibili fin dal 1930-35. In alcuni paesi come in Gran Bretagna e negli stati Uniti l’abbondono dell’amianto navale, in particolare della crocidolite spruzzata, inizia a metà degli anni ’60, più precocemente che in altri paesi ed in Italia. Vale la pena richiamare che l’amianto una volta applicato rimane in situ a futura memoria, disponibile, se non adeguatamente controllato, all’esposizione di marinai, viaggiatori, manutentori, ristrutturatori e poi di bonificatori.
I siti degli stabilimenti navali più̀ estesi, ora di proprietà̀ Fincantieri e, in passato, imponenti utilizzatori di amianto, sono: Monfalcone, quello di dimensioni maggiori, Marghera, Sestri Ponente, Riva Trigoso, Muggiano, Ancona, Castellammare di Stabia e Palermo. Esistevano anche altri cantieri navali, spesso di dimensioni minori e attualmente dismessi oppure non acquisiti da Fincantieri, a Trieste, Livorno, Civitavecchia, Napoli, Messina, Genova, La Spezia, Ancona, Ravenna, Pesaro, Venezia. In passato gli organici erano molto consistenti, complessivamente tutti i cantieri italiani nel 1975 occupavano direttamente oltre ventunomila addetti che diventano neanche dodicimila nel 1990. Agli stabilimenti civili, è necessario aggiungere quelli dell’Arsenale militare marittimo di Taranto e di La Spezia che attualmente occupano oltre duemila dipendenti ciascuno, in maggioranza civili.
Per rendere conto delle condizioni di lavoro, e non solo, nell’era dell’amianto Alessandro Morena, uno storico ha intervistato i diretti interessati, un tecnico della sicurezza, degli operai ed una inserviente alla mensa del cantiere di Monfalcone producendo così informazioni utilissime e di grande effetto.
La prima tappa delle ricerche degli effetti più temibili dell’amianto delle navi è rappresentata da un’osservazione fatta negli ospedali di Trieste negli anni ’50 e ’60; si rileva che un tipo di tumore fino a quel tempo ritenuto assai raro, il mesotelioma maligno della pleura, vien diagnosticato con una frequenza del tutto inaspettata. Nel 1973 viene pubblicato lo studio relativo a 20 casi di mesotelioma maligno della pleura, diagnosticati sempre a Trieste tra il novembre 1967 e il novembre 1971, 13 di questi avevano lavorato nell’industria navale. Negli stessi anni procedono gli interventi nei cantieri navali di Trieste e quindi le ricerche dell’Istituto di medicina del lavoro di Trieste. L’articolo Cancro da lavoro a Trieste: il mesotelioma della pleura, pubblicato nel 1976 sulla rivista di divulgazione scientifica Sapere, conclude questa fase di studi scientifici; gli autori sono consapevoli, e lo comunicano a chiare lettere, degli effetti presenti e futuri dell’uso dell’amianto nell’area che interessa tre comparti produttivi principali, la navalmeccanica, il porto e la Grandi Motori, dove erano stati individuati 65 casi di mesoteliomi fra i lavoratori.
In Liguria l’attenzione all’impatto dell’amianto sui lavoratori portuali e dei cantieri navali era stata già posta in forma allarmante nel 1971 con un lavoro che illustra una casistica studiata negli ultimi quattro anni di attività̀ dell’Istituto di Medicina del Lavoro dell’Università̀ di Genova e della Divisione di Medicina del Lavoro dello Ospedale S. Martino, un numero relativamente elevato di ammalati di asbestosi a seguito di una attività̀ professionale svolta più̀ o meno a lungo nei cantieri navali di La Spezia e di Genova; tra questi sono stati registrati nove casi di tumori maligni dell’apparato respiratorio, 8 tumori polmonari ed 1 mesotelioma pleurico.
Nel registro italiano ReNaM sono iscritti 1184 mesoteliomi tra i lavoratori dei cantieri navali, 490 in Liguria, 276 nel Friuli Venezia Giulia e 69 nelle Marche. Tra gli addetti alla riparazione e demolizione di natanti i casi registrati sono 271 e di questi 156 in Liguria, 47 in Toscana e 16 in Sicilia.
——————
* Francesco (Franco) Carnevale è medico del lavoro pubblico attivo prima all’Università di Padova e di Verona e poi nell’ambito del Sistema sanitario regionale toscano, a Firenze. Coltiva la storia della salute dei lavoratori. E’ autore di Mal da lavoro. Storia della salute dei lavoratori, Laterza, Roma-Bari 1999, di Malati di lavoro. Artigiani e lavoratori, medicina e medici da Bernardino Ramazzini a Luigi Devoto (1770-1900), Polistampa, Firenze 2015 (in collaborazione con Alberto Baldasseroni) e di Annotazioni al Trattato delle malattie dei lavoratori di Bernardino Ramazzini, Polistampa, Firenze 2016